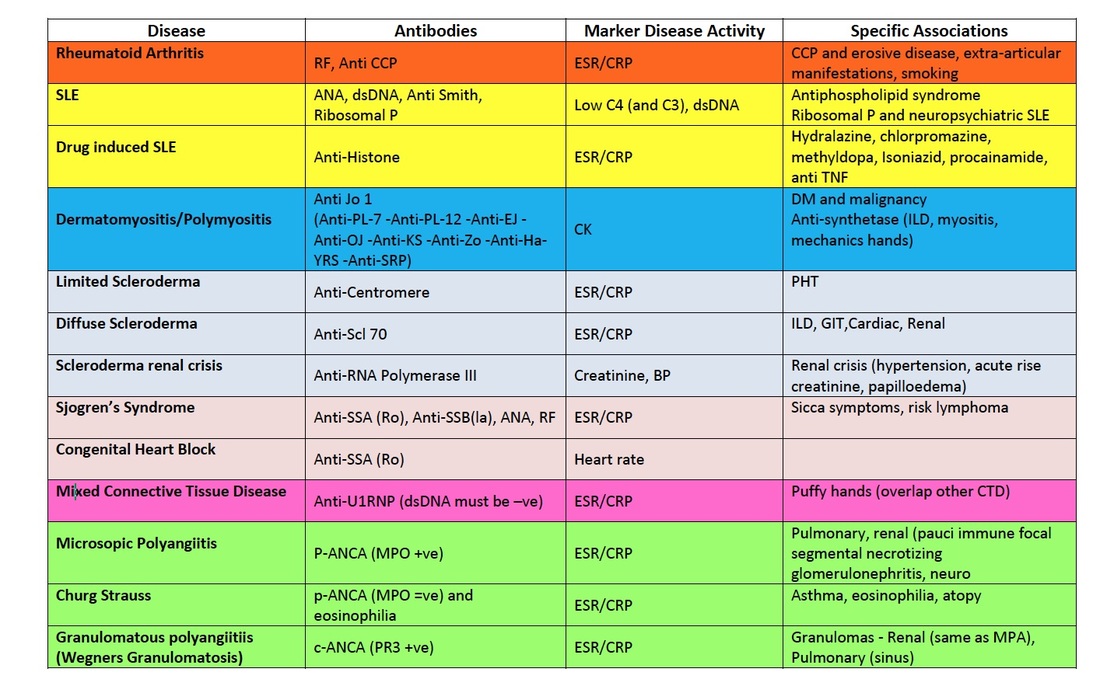
Antibodies in Rheumatology
Rheumatoid Arthritis
Stem: This patient presented with painful hands. Please examine him
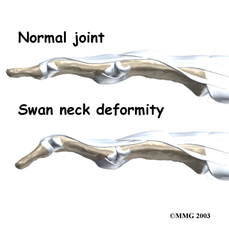
Presentation: I reviewed Mr RJ, a gentleman with painful hands (repeat the stem back). The most pertinent findings include a destructive symmetrical polyarthropathy of the hands involving the proximal interphalangeal joints and metacarpophalangeal joints with sparing of the distal phalangeal joints, ulnar deviation of the fingers, volar subluxation at the metacarpophalangeal joints, swan neck deformity and Z-deformity of the thumb, rheumatoid nodules at the elbow and fine end-inspiratory crackles at the bases of the lung with a moderate sized left sided pleural effusion. Her grip strength, pincer strength and opposition were limited (functional assessment). This is consistent with erosive nodular rheumatoid arthritis complicated by interstitial lung disease. In detail there were no features of cushings syndrome. She had a destructive symmetrical polyarthropathy involving the proximal interphalangeal joints (avoid abbreviations) and metacarpophalangeal joints, with ulnar deviation at the carpometacarpal joints and volar subluxation at the metacarpophalngeal joints. She had evidence of Z-deformity of the thumb and the swan neck deformity. She had sparing of the distal interphalangeal joints. There was no evidence of flexor tenosynovitis or trigger fingers, and there was no tendon crepitus. She had rheumatoid nodules on the extensor surfaces of her elbows. Her range of movement was limited bilaterally, most notably flexion and extension at the metacarpophalangeal joints. Her functional strength was limited with reduced grip strength, finger opposition and pincer strength. She had difficulty in unscrewing the jar and manipulating the key. Extra-articular examination revealed no evidence of scleritis, episcleritis or scleromalacia perforans (mention important negatives). She had evidence of an interstitial lung process with fine end-inspiratory crackles at both lung bases and percussion dullness at the left lung base suggesting a pleural effusion.
You mention swan neck deformity, Z deformity and boutonniere's deformity, please show me where they are and describe the anatomical changes.
Presentation: I reviewed Mr RJ, a gentleman with painful hands (repeat the stem back). The most pertinent findings include a destructive symmetrical polyarthropathy of the hands involving the proximal interphalangeal joints and metacarpophalangeal joints with sparing of the distal phalangeal joints, ulnar deviation of the fingers, volar subluxation at the metacarpophalangeal joints, swan neck deformity and Z-deformity of the thumb, rheumatoid nodules at the elbow and fine end-inspiratory crackles at the bases of the lung with a moderate sized left sided pleural effusion. Her grip strength, pincer strength and opposition were limited (functional assessment). This is consistent with erosive nodular rheumatoid arthritis complicated by interstitial lung disease. In detail there were no features of cushings syndrome. She had a destructive symmetrical polyarthropathy involving the proximal interphalangeal joints (avoid abbreviations) and metacarpophalangeal joints, with ulnar deviation at the carpometacarpal joints and volar subluxation at the metacarpophalngeal joints. She had evidence of Z-deformity of the thumb and the swan neck deformity. She had sparing of the distal interphalangeal joints. There was no evidence of flexor tenosynovitis or trigger fingers, and there was no tendon crepitus. She had rheumatoid nodules on the extensor surfaces of her elbows. Her range of movement was limited bilaterally, most notably flexion and extension at the metacarpophalangeal joints. Her functional strength was limited with reduced grip strength, finger opposition and pincer strength. She had difficulty in unscrewing the jar and manipulating the key. Extra-articular examination revealed no evidence of scleritis, episcleritis or scleromalacia perforans (mention important negatives). She had evidence of an interstitial lung process with fine end-inspiratory crackles at both lung bases and percussion dullness at the left lung base suggesting a pleural effusion.
You mention swan neck deformity, Z deformity and boutonniere's deformity, please show me where they are and describe the anatomical changes.
What is the mechanism of the pseudobenediction sign in rheumatoid arthritis?
It occurs when the damaged ulnar styloid compresses and ruptures the extensor tendons of the 4th and 5th digits, leading to inability to extend the 4th and 5th digit
Are you sure that these nodules you found are rheumatoid in nature? What is your differential diangosis for these nodules
In the context of typical rheumatoid features, I believe that the most likely aetiology for the nodules are rheumatoid nodules. The differential diagnosis includes cutaneous sarcoidosis, granuloma annulare, gouty tophi and tendon xanthoma. Histology of these nodules would show diffuse pallisading and/ or interstitial granulomatous inflammation. They are almost always associated with sero-positive disease. J Cutan Pathol. 2003 Jan;30(1):1-10.
You mentioned that the patient had a trigger finger. Explain the pathophysiology with respect to the underlying diagnosis.
Tenosynovitis, which is very common in rheumatoid arthritis, causes thickening and nodule formation on the flexor tendon sheath. These nodules get entrapped at the pulley's present on the flexor surface, for example the A1 pully, resulting in a flexion deformity of the finger.
What are the clinical signs that you may see in the eye in a patient with rheumatoid arthritis?
Episcleritis, scleritis, scleromalacia perforans, dry eyes (secondary sjogrens syndrome), steroid induced cataracts, chloroquine induced corneal deposits or retinopathy
What are the diagnostic criterion used for rheumatoid arthritis?
The American College of Rheumatology (2010 ACR-EULAR) have a set of newly revised diagnostic criterion. There are 4 broad criterion (1) Number of joints involved (2) Serology (RF +/- ACPA) (3) Acute phase response (ESR +/- CRP) and (4) duration of symptoms (>6 weeks). There are a total of 10 points, of which greater than 6 are required for a diagnosis
What is a rheumatoid factor?
Rheumatoid factor is an antibody, typically IgM directed against the constant region of human immunoglobulins. It is only found in ~ 75% of RA (therefore sero-negative RA), and can be found in other diseases such as SLE, sjogren's syndrome, cryoglobulinaemic vasculitis. Furthermore, a significant percentage of the normal population (~5%) have normal RF. It is an adverse prognostic marker, associated with aggressive, erosive disease with extra-articular manifestations. RF does not reflect disease actvity - Dis Markers. 2013; 35(6): 727–734.
Briefly discuss the pathophysiology of Rheumatoid arthritis
- HLA DR1/4 related, unknown aetiology, concept of shared epitope [on 3rd hypervariable region, determines way antigens are presented, 5 amino acids that confer susceptibility]
- Citrullination: enzyme peptidyl arginine deaminase that converts arginine to citrulline more stable in Ra sufferers, this causes neo-epitopes, confers risk of RA, smoking increases this as it also causes citrullination in alveoli
Suppose you aspirate the pleural effusion, what is the biochemistry that you expect to see?
Very low glucose, low pH and presence of RF - N Engl J Med 2002; 346:1971-1977
What is palindromic rheumatism and why is it important to recognise?
It is a sudden onset large joint, non destructive migratory arthropathy that is exquisitely sensitive to hydroxychloroquine.
What are adverse prognostic markers?
- erosive disease (marrow oedema on MRI signifies increased likelihood of developing erosions
- RF +
- ACPA + (> RF)
- Involved joint count
What are the radiological features of rheumatoid arthritis?
- joint space narrowing (uniform in comparison to OA)
- joint erosions
- peri-articular soft tissue swelling
- juxta-articular joint osteoporosis
It occurs when the damaged ulnar styloid compresses and ruptures the extensor tendons of the 4th and 5th digits, leading to inability to extend the 4th and 5th digit
Are you sure that these nodules you found are rheumatoid in nature? What is your differential diangosis for these nodules
In the context of typical rheumatoid features, I believe that the most likely aetiology for the nodules are rheumatoid nodules. The differential diagnosis includes cutaneous sarcoidosis, granuloma annulare, gouty tophi and tendon xanthoma. Histology of these nodules would show diffuse pallisading and/ or interstitial granulomatous inflammation. They are almost always associated with sero-positive disease. J Cutan Pathol. 2003 Jan;30(1):1-10.
You mentioned that the patient had a trigger finger. Explain the pathophysiology with respect to the underlying diagnosis.
Tenosynovitis, which is very common in rheumatoid arthritis, causes thickening and nodule formation on the flexor tendon sheath. These nodules get entrapped at the pulley's present on the flexor surface, for example the A1 pully, resulting in a flexion deformity of the finger.
What are the clinical signs that you may see in the eye in a patient with rheumatoid arthritis?
Episcleritis, scleritis, scleromalacia perforans, dry eyes (secondary sjogrens syndrome), steroid induced cataracts, chloroquine induced corneal deposits or retinopathy
What are the diagnostic criterion used for rheumatoid arthritis?
The American College of Rheumatology (2010 ACR-EULAR) have a set of newly revised diagnostic criterion. There are 4 broad criterion (1) Number of joints involved (2) Serology (RF +/- ACPA) (3) Acute phase response (ESR +/- CRP) and (4) duration of symptoms (>6 weeks). There are a total of 10 points, of which greater than 6 are required for a diagnosis
What is a rheumatoid factor?
Rheumatoid factor is an antibody, typically IgM directed against the constant region of human immunoglobulins. It is only found in ~ 75% of RA (therefore sero-negative RA), and can be found in other diseases such as SLE, sjogren's syndrome, cryoglobulinaemic vasculitis. Furthermore, a significant percentage of the normal population (~5%) have normal RF. It is an adverse prognostic marker, associated with aggressive, erosive disease with extra-articular manifestations. RF does not reflect disease actvity - Dis Markers. 2013; 35(6): 727–734.
Briefly discuss the pathophysiology of Rheumatoid arthritis
- HLA DR1/4 related, unknown aetiology, concept of shared epitope [on 3rd hypervariable region, determines way antigens are presented, 5 amino acids that confer susceptibility]
- Citrullination: enzyme peptidyl arginine deaminase that converts arginine to citrulline more stable in Ra sufferers, this causes neo-epitopes, confers risk of RA, smoking increases this as it also causes citrullination in alveoli
Suppose you aspirate the pleural effusion, what is the biochemistry that you expect to see?
Very low glucose, low pH and presence of RF - N Engl J Med 2002; 346:1971-1977
What is palindromic rheumatism and why is it important to recognise?
It is a sudden onset large joint, non destructive migratory arthropathy that is exquisitely sensitive to hydroxychloroquine.
What are adverse prognostic markers?
- erosive disease (marrow oedema on MRI signifies increased likelihood of developing erosions
- RF +
- ACPA + (> RF)
- Involved joint count
What are the radiological features of rheumatoid arthritis?
- joint space narrowing (uniform in comparison to OA)
- joint erosions
- peri-articular soft tissue swelling
- juxta-articular joint osteoporosis
Psoriatic Arthritis
Stem: This patient presents with a rash and difficulty using her hands. Please examine her.
I reviewed Mrs XA, a 46 y female witha rash and difficulty using her hand. The most significant findings include a symmetrical polyarthropathy sparing the distal interphalangeal joint but involving the proximal interphalangeal joint and metacarpophalangeal joints, dactylitis, nail pitting, transverse ridging and subungal hyperkeratosis with onycholysis, achilles tendon enthesitis and plantar fasciitis. There is a erythematous, white scaly rash on the extensor surfaces of the elbows and following the scalp line posteriorly. Hand grip, opposition and pincer strength was markedly reduced as a result of her arthropathy. The diagnosis is psoriatic arthropathy. In detail, the patient appeared comfortable sitting in bed. There was no evidence of cushingoid features. As mentioned, there is a symmetrical small joint polyarthropathy sparing the distal interphalagneal joints. Nail changes have already been mentioned. There is evidence of dactylitis. There was no evidence of palmar erythema or entrapment neuropathy. There was evidence of wasting of the intrinsic muscles of the hands. There was reduced grip strength, pincer grip and opposition. She was unable to perform the jar opening functional test. Prominent psoriatic scars were noted over the extensor surfaces of both arms. There was no evidence of rheumatoid nodules. There was no evidence of aortic regurgitation. Examination of the feet revealed achilles tendonitis and plantar fasciitis.
What are the 5 different manifestations or patterns of psoriatic arthropathy
Can arthritis precede psoriasis?
Yes. In 20% of patients, the arthropathy precedes the typical skin rash, and can occur as much as 20 years prior to the arthropathy. 5 - 8% of patients with skin manifestations may develop psoriatic arthropathy.
What is the koebner phenomenon?
This relates to the fact that trauma or surgery over a specific region triggers the psoriatic skin rash within this region. The deep koebner phenomenon relates to the fact that injury over a specific superficial area triggers arthritis at the joints peripherally injured
Is there any genetic predisposition to develop psoriatic arthropathy?
Yes, 40% of patients with PsA have first degree relatives that are affected. There is a HLA-B27 association, however it is weaker in association than ASpA.
What are the nail changes that are seen in psoriatic arthropathy?
onycholysis, subungal hyperkeratosis, transverse ridging and nail pitting - the degree of which correlates with the liklihood of having PsA
How can you differentiate Rheumatoid arthritis from psoriatic arthritis?
I reviewed Mrs XA, a 46 y female witha rash and difficulty using her hand. The most significant findings include a symmetrical polyarthropathy sparing the distal interphalangeal joint but involving the proximal interphalangeal joint and metacarpophalangeal joints, dactylitis, nail pitting, transverse ridging and subungal hyperkeratosis with onycholysis, achilles tendon enthesitis and plantar fasciitis. There is a erythematous, white scaly rash on the extensor surfaces of the elbows and following the scalp line posteriorly. Hand grip, opposition and pincer strength was markedly reduced as a result of her arthropathy. The diagnosis is psoriatic arthropathy. In detail, the patient appeared comfortable sitting in bed. There was no evidence of cushingoid features. As mentioned, there is a symmetrical small joint polyarthropathy sparing the distal interphalagneal joints. Nail changes have already been mentioned. There is evidence of dactylitis. There was no evidence of palmar erythema or entrapment neuropathy. There was evidence of wasting of the intrinsic muscles of the hands. There was reduced grip strength, pincer grip and opposition. She was unable to perform the jar opening functional test. Prominent psoriatic scars were noted over the extensor surfaces of both arms. There was no evidence of rheumatoid nodules. There was no evidence of aortic regurgitation. Examination of the feet revealed achilles tendonitis and plantar fasciitis.
What are the 5 different manifestations or patterns of psoriatic arthropathy
- Monoarthritis or asymmetric oligoarthritis with DIPJ involvement
- DIPJ arthritis with nail bed changes - classical presentation, but not the most common
- Symmetrical polyarthritis sparing the DIPJs - MRCP paces book suggests this is the most common
- arthritis mutilans
- Spondylitis +/- sacroilitis
Can arthritis precede psoriasis?
Yes. In 20% of patients, the arthropathy precedes the typical skin rash, and can occur as much as 20 years prior to the arthropathy. 5 - 8% of patients with skin manifestations may develop psoriatic arthropathy.
What is the koebner phenomenon?
This relates to the fact that trauma or surgery over a specific region triggers the psoriatic skin rash within this region. The deep koebner phenomenon relates to the fact that injury over a specific superficial area triggers arthritis at the joints peripherally injured
Is there any genetic predisposition to develop psoriatic arthropathy?
Yes, 40% of patients with PsA have first degree relatives that are affected. There is a HLA-B27 association, however it is weaker in association than ASpA.
What are the nail changes that are seen in psoriatic arthropathy?
onycholysis, subungal hyperkeratosis, transverse ridging and nail pitting - the degree of which correlates with the liklihood of having PsA
How can you differentiate Rheumatoid arthritis from psoriatic arthritis?
|
Rheumatoid arthritis
|
Psoriatic arthritis
|
I agree that this patient does indeed have dactylitis. What does it represent and are there any other conditions that you know of that may present with dactylitis?
Dactylitis manifests physically as soft tissue swelling of an entire digit. The pathological basis is tenosynovitis and soft tissue inflammation. Conditions that manifest with dactylitis include spondyloarthritis, rheumatoid arthritis, tuberculosis, syphilis - (Boston Med Surg J 1872; 86:303-305), sarcoidosis, sickle cell disease. With regards to the pathophysiological mechanism, it has been hypothesised that in sponyloarthritis, the primary insult of enthesitis causes diffusion of pro-inflammatory cytokines along the tenosynovial sheath therefore triggering inflammation.
Dactylitis manifests physically as soft tissue swelling of an entire digit. The pathological basis is tenosynovitis and soft tissue inflammation. Conditions that manifest with dactylitis include spondyloarthritis, rheumatoid arthritis, tuberculosis, syphilis - (Boston Med Surg J 1872; 86:303-305), sarcoidosis, sickle cell disease. With regards to the pathophysiological mechanism, it has been hypothesised that in sponyloarthritis, the primary insult of enthesitis causes diffusion of pro-inflammatory cytokines along the tenosynovial sheath therefore triggering inflammation.
What are the extra-articular manifestations of spondyloarthritis?
- Nails - as described above in psoriatic arthritis
- Enthesitis
- Anterior uveitis
- colitis - note that 70% of patients who have ASpA have asymptomatic colitis on colonoscopy
- Aortic regurgitation and aortitis
- Apical fibrosis
- Secondary amyloidosis - leads to nephrotic syndrome
- Neurological symptoms - cauda-equina, vertebral fractures
Ankylosing Spondylitis
General Inspection
Investigations
- Question mark posture seoncary to loss of cervical and lumbar lordosis with exaggeration of thoracic kyphosis
- Increased because of ankylosing of the spine and thoracic kyphyosis which is unable to be correted via normal thoracic extension --> fixed flexion deformity of upper (thoracic) spine
- Normally should be able to touch the occiput to the wall
- Eponymously named Flesche's test
- Tests extent of lumbar flexion, which is decreased in ankylosing spondylitis (<5cm)
- Unlike mechanical spinal disease, ankylosing spondylitis will show symmetrical decrease in spinal movements at the level of the cervical spine (rotational, flexion, extension, side flexion and side extension), thoracic spine (rotation upon sitting down at the bed, chest expansion <4cm) and lumbar spine (flexion via the modified shober's test, extension)
- Chest expansion is mainly reduced secondary to spinal disease but apical fibrosis can also contribute
- Radiology of spinal disease:
- Squaring of the vertebral bodies
- syndesmophytes, ankylosis of the facet joints, and calcification of the anterior longitudinal ligament
- bamboo spine
- Tenderness secondary to sacro-ilitis
- Radiologically graded: Grade 0 - normal, Grade 1 - suspicious changes, Grade 2 - minimal abnormality – small localized areas with erosions or sclerosis, without alteration in the joint width, Grade 3 - unequivocal abnormality – moderate or advanced sacroiliitis with one or more of the following: erosions, evidence of sclerosis, widening, narrowing, or partial ankylosis, Grade 4 - total ankylosis
- Definite sacroilitis if bilateral grade 2 or unilateral grade 3
- MRI --> "bone marrow oedema" which is a hyperintense signal in the bones adjacent to the affected joints
- Aortic regurgitation
- Mitral valve prolapse
- Anterior uveitis (slit lamp examination)
- Painful red eye, photophobia, blurred vision
- Requires demonstration of inflammation in the anterior chamber of the eye
- Achilles tendonitis, plantar fasciitis
- all manifestations of enthesitis
- Peripheral large joint oligoarthritis
- Hip arthritis – most common ‘peripheral’ joint
- Atlanto-axial subluxation
- Cauda-equina syndrome (rarely)
- Amyloidosis
- atrioventricular conduction delay
- Apical fibrosis
- usually asymptomatic, chest wall restriction secondary to arthritis of the costo-vertebral joints is more of a problem
- Dactylitis
- Inflammatory bowel disease
- note that 70% of patients who have ASpA have asymptomatic colitis on colonoscopy
Investigations
- Spinal imaging
- look for squaring of vertebrae, romanus lesion, syndesmophytes, calcification of the anterior longitudinal ligament
- flex/ ext views of cervical spine to look for atlanto-axial subluxation
- SI Joint imaging
- Grades of sacroiilitis as described above
- FBC/ CRP/ ESR
- Markers of inflammation and disease activity
- normochromic normocytic anaemia - of chronic disease
- HLA-B27
- 90% of patients with ankylosing spondylitis have HLA-B27
- But ankylosing spondylitis is present in only 8% of patients with HLA-B27
- UEC
- renal dysfunction in secondary amyloidosis
- MRI
- Early changes suggestive of bone marrow oedema
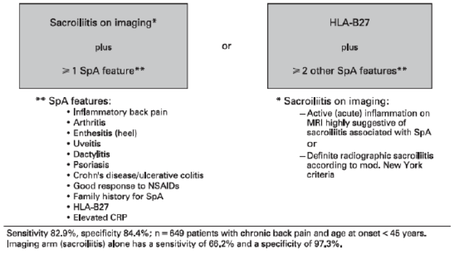
- Based on modified new york criterion requires one clinical manifestation (essentially demonstrating inflammatory back pain or reduced spinal movements) and radiological manifestations (bilateral grade 2 sacroilitis or unilateral grade 3/ 4 sacroilitis) but radiographic sacroilitis takes years to develop.
- See below image for alternative criterion:
Gout
- Feet - Metatarsophalangeal joint of the great toe involved in 75% of cases
- Ankles & Knees – Involved after recurrent attacks
- Fingers, Wrists and Elbows - affected late
- Gouty Tophi = Urate deposits with surrounding inflammatory cells [Latin tophus, 'chalk stone']. Presence = Chronic Recurrent Gout
- Joint synovia
- Olecranon bursa
- Extensor surface of the forearm
- Helix of the ear
- Infrapatellar & Achilles tendons
- (Urate deposits with inflammatory cells surrounding them [Latin tophus, 'chalk stone']
What are the types of crystals that can be found in synovial fluid?
- Monosodium urate monohydrate = acute gout, tophaceous gout
- Calcium pyrophosphate dehydrate = spectrum, acute pseudogout, destructive arthropathy, asymptomatic
- Basic calcium phosphate = Milwaukee shoulder
- Calcium oxalate = acute arthritis
- Lipid = acute arthritis
What is the pathophysiology of gout
- There is an imbalance between production of urate and clearance of urate, with subsequent supersaturation of uric acid crystals, activation of the inflammasome and local inflammation
- Production: genetic due to PrPP synthetase mutation, acquired due to myeloproliferative disease, high intake, alcohol, obesity, high trigs. 1/3 from diet, 2/3 endogenous
- Urate produced from purines (dietary = red meat, seafood, bacon, dairy and coffee protective, alcohol = beer>wine>spirits, endogenous), oestrogen reduces hyperuricaemia therefore less incidence in females cf males, transplant (tacro and cyclosporine are risk factors)
- Clearance: genetic due to HRPT mutation, renal disease
- Urate crystal supersaturation [note in 49% hyperuricaemia absent] + nucleating factors (seed from fragment of cartilage, debris) + favourable factors (decr pH, cold, decreased hydration of cartilage) causes crystallisation subsequently leading to activation of inflammasome and IL-1 beta secretion, phagocyte recruitment, inflammation and release of cytokines (IL6, TNF-alpha)
What are the radiological changes associated with chronic tophaecous gout?
- Swelling, eccentric opacities, well preserved joint space, punched out erosions with sclerotic margins and overhanging edges
- Can use Dual energy CT scan, especially if difficult to aspirate, can show difference between urate and calcium pyrophosphate
How would you treat acute gout?
- NSAIDs: need dose upper limit of normal, normal CIs for NSAIDS exist
- Colchicine: disrupts microtubule fx, low dose is equivalent to high dose with less SE, use in acute situation, long term SE = neuromyopathy in renal impairment
- Systemic corticosteroid = need 30 – 50mg for 5d
- Depot ACTH (40mg IM)
- Intra-articular corticosteroid = req technical competence, skin atrophy at site of inj, rapid onset of action, well tolerated
- Canakinumab (IL-1b) in an RCT, good evidence coming, licensed in EU --> targets inflammasome mechanism
- Anakinra: IL-1R antagonist, shorter half life than canakinumab --> targets inflammasome mechanism
How would you treat chronic tophaceous gout?
- Symptom control/suppression – colchicine can be used 0.5mg daily, EMG/ NCS mild axonopathy, myoneuropathy risk, low dose oral corticosteroids
- Reduce urate load, aim <0.36mM: Indication for Rx with hyperuricaemia + gouty arthritis (tophi, erosions, >2 attacks/yr, urate nephropathy, urate calculi), NOT Rx if asymptomatic and non of the aforementioned as toxicity to great and evidence of benefit lacking
- Allopurinol inhibits xanthine oxidase, start low, dose 100 – 800mg. Treat to target by reducing urate load
- risk of hypersensitivity [HLAB5801, occurs <6w into dose, causes DRESS (Drug rash with eosinophilia and systemic symptoms + interstitial nephritis + hepatitis)
- Feboxistat, now licensed, non purine analogue inhibitor of xanthine oxidase --> allopurinol allergy pts
- Uricosouric agents --> effectively inhibit uric acid reabsorption in prox tubule [URAT1/ OAT4 inhibition] eg probenecid + losartan
Osteoarthritis
- Asymmetrical bony swelling on DIPJ = Heberden's nodes, PIP = bouchard's nodes - these are tender osteophytic extensions of the joint
- 1st MCP often involved, especially in females
- Varus deformity in knee more common in OA because the medial compartment is affected more frequently
- Assess for knee effusion
- Crepitus during passive motion of the knee
- Antalgic gait
- See long case section for further information
Systemic Sclerosis
- General Inspection
- Bird-like facies
- Weight-loss (malabsorption)
- Alopecia
- Hands
- Pigmentation
- Fixed flexion deformities/contractures
- Loss of distal pulps
- Digital pitting +/- ulceration
- Periungual changes (subungual erythema)
- Nailfold abnormalities
- Telangiectasia
- Sclerodactyly
- Rayauds
- Calcinosis
- Wrists/MCP/PIP/DIP tenderness (20% have synovitis)
- Flexor tendons – friction rubs
- Ulnar and Radial pulses
- Capillary return
- Skin thickening
- Elbows (calcinosis and nodules to exclude overlap syndrome)
- Arms
- Skin thickening/tightening
- Limited (face + <elbows/knees) or
- Diffuse (>elbows/knees or torso/chest/back involved)
- BP – renal crisis
- Hair loss
- Proximal myopathy (normal CK myositis)
- Head (bird like facies)
- Alopecia
- Eyes:
- Eyebrows lost
- Pull eyelids down (tightening)
- Conjunctival pallor (anaemia)
- Dry mouth (Sjogrens)
- Puckered mouth
- Narrow aperture – 3 finger test
- Telangiectasia – inside lower lip
- Mouth ulcers – MTX
- Sip Test – Oesophageal dysmotility
- Chest
- Tight Skin (Systemic Sclerosis)
- RV heave/palpable P2 Pulmonary HTN, JVP, TR
- Bases – fine inspiratory crepitations
- Lower Limbs
- Skin thickening - extent
- Small joint arthropathy
- Vasculitis
What are the disease manifestations of Scleroderma?
- Arthralgia is reported in 98% [erosive in 25%], Tenosynovitis with tendon friction rub
- Myalgia --> muscle biopsy would probably show fibrosis, CK typically negative in this disease
- GIT --> eosophageal hypomotility, gastric antral vascular ectasia, GI involvement portends a very poor prognosis
- Interstitial Lung Disease:
- DLCO<50 assoc with worse prognosis and assoc with pulm HTN, progression occurs early in on the course of the disease [first 5y], Scl70 predictor of getting disease, anti-centromere protective, histology = NSIP (90%)> UIP [worse] pattern, in fact HRCT is most powerful predictor of mortality
- Dx --> HRCT, DLCO, 6 min walk test
- Rx --> cyclophosphamide for 12/12, BMTx trials St Vincents, RPAH
- DLCO<50 assoc with worse prognosis and assoc with pulm HTN, progression occurs early in on the course of the disease [first 5y], Scl70 predictor of getting disease, anti-centromere protective, histology = NSIP (90%)> UIP [worse] pattern, in fact HRCT is most powerful predictor of mortality
- Pulmonary Hypertension:
- Occurs in 12% of patients with both limited and diffuse disease
- Later complication: 5-10 years of duration of disease
- Dx suspected when DLCO <50% with minimal fibrosis on HRCT, ECHO shows RV-RA > 50mmHg, indicated to proceed to RH catheter study
- Mean pulmonary artery pressure > 25mmHg with PCWP < 18mmHg
- Mean PAP on exercise > 30mmHg with wedge < 18mmHg
- Rx
- Mainstay now is combination therapy include endothelin antagonists, PDE5 inhibitors and prostaglandins but single agent therapy only subsidized in Australia, and must show clinical stability in 6/12 for ongoing Rx
- Ambrisentan + tadalafil cf monotherapy reduced Rx failure by 50% in particular hospitalisations
- Rx only subsidized for WHO functional class III or IV
- Mainstay now is combination therapy include endothelin antagonists, PDE5 inhibitors and prostaglandins but single agent therapy only subsidized in Australia, and must show clinical stability in 6/12 for ongoing Rx
- Cardiac disease: fibrosis, conduction deficits, coronary spasm, assoc with diffuse disease + Scl-70, effusions in 30 – 40%
- Renal disease: hypertensive crisis, secondary to microvacular changes, assoc with RNA polymerase antibodies, renal crisis assoc with HTN + oliguric renal failure, use ACE-inhibitors
Dermatomyositis
Examination features
- Proximal muscle weakness and/or pain
- Skin rash = heliotrope rash, shawl sign, gottron’s papules [pathomnemonic, erythematous rash over MCP and PIPJ], dilated nailfold capillaries, mechanics hands, interstitial lung disease
- Suspect based on clinical Hx
- CK, aldolase --> but maybe normal
- ANA+, ENA --> Jo1 = tRNA synthetase Abs (more for polymyositis but occurs in Dermatomyositis), Mi-2 (highly specific), TIF-1-gamma --> Dermatomyositis + malignancy
- EMG --> myopathic features (increased insertional activity, fibrillations, myopathic low amplitude, polyphasic potentials, complex repetitive discharges)
- Muscle biopsy --> gold standard
- MRI: T1 demonstrates atrophy, T2 shows muscle oedema, can guide where to biopsy if no obvious weak muscle present
- Malignancy --> 15% incidence, screen for common things
- Glucocorticoids 1mg/kg <80mg/d, if severely ill pulse methylpred 1g/d 3/7
- Start steroid sparing agent at same time à MTX/AZA, AZA better if there is ILD in association
- IVIG has some promise