Osteoarthritis
Aust Prescr 2015;38:115-9
History
History
- Quantifying the number of joints involved
- The nature of the pain - trying to delineate the difference between inflammatory and non-inflammatory arthropathy (eg morning stiffness, gel phenomenon)
- Effect on function
- Risk factors - age, obesity, heritable, osteoporosis is protective, secondary osteoarthritis can occur secondary to trauma, bony deformities, inflammatory arthropathy
- 50% radiological, 12% symptomatic. Implies radiology does not equate to symptoms
- Disease of articular cartilage --> progressive loss
- Bouchards/ heberdens, varus, joint tenderness, effusions, trendelemburgs, antalgic gait
- Clinical Dx supported by radiology
- Normal inflammatory markers
- Synovial fluid has high viscosity, cell count <2000
- Imaging. X-ray (joint space narrowing, subchondral sclerosis, bony cysts, osteophytes), MRI after X-ray [bone marrow lesions = sclerotic but poorly mineralized bones, predict pain, cartilage damage and loss]
- Goals of Management:
- short term - to acutely manage pain
- medium and long term - improve functionality and mobility with improvements in quality of life
- Non pharmacological
- Exercise is universally recommended by clinical guidelines, and should be individualised after patient assessment
- Exercise has small to moderate effect sizes for improved function and pain relief, similar to those achieved with non-steroidal anti-inflammatory drugs (NSAIDs) and analgesia
- If there are functional and mobility limitations then I would pursue water based exercise regimes
- Targeted muscle exercises and aerobic exercises are generally recommended
- Stretching and flexibility exercises generally form part of an overall exercise program for osteoarthritis, to maintain or increase the range of motion in the joints
- Supervised exercises are better than individualised exercises with regards to pain reduction
- Mobility aids such as a stick (used in the opposite hand), knee braces and foot orthoses can also diminish pain and improve function
- Weight loss, as obesity is an important modifiable risk factor, 50% improvement in symptoms with 10% weight reduction through diet and exercise
- Pharmacological
- NSAIDS first line, efficacy is superior to paracetamol, combine with PPI if concerned - reduces dyspepsia by 66%
- A meta-analysis of 26 studies comparing the two found that COX-2 inhibitors reduced the relative risk of dyspepsia by 12% and the absolute risk by 3.7%
- Paracetamol no greater than placebo for knee arthritis, lower effect than NSAIDS, and safety concerns arising with regard to GI and multi-organ dysfunction
- Topical NSAIDS - applied 3 - 4 times a day, works for knee and hand osteoarthritis, local drug delivery reduces GI side effects. An example is topical diclofenac sodium 1% gel. Topical capsaicin can also be used
- Intra-articular injections - provide short-term pain relief (1–2 weeks in randomised controlled trials) and improved function for patients with osteoarthritis, intra-articular injections given more frequently than once every four months can result in cartilage and joint damage.
- Opioids - alternative for patients who cannot tolerate or be prescribed first-line drugs
- Joint replacement surgery should be considered for severe clinical disease with inadequate response to conservative treatment.
Lumbar Spinal Canal Stenosis
BMJ 2016;352:h6234
General Information
General Information
- degenerative condition in which changes in the discs, ligamentum flavum, and facet joints with aging cause narrowing of the spaces around the neurovascular structures of the spine
- Most common indication for spinal surgery for age > 65
- facet joint hypertrophy, loss of intervertebral disc height, disc bulging, osteophyte formation, and hypertrophy of the ligamentum flavum
- extension of the lumbar spine reduces the size of the lumbar spinal canal, as does axial loading
- Neurogenic claudication symptoms
- progressive onset of pain, numbness, weakness, and tingling in the low back, buttocks, and legs, which is initiated by standing, walking, or lumbar extension
- shopping cart sign - patient walking in a flexed or stooped position to relieve or reduce symptoms
- DDx vascular claudication - exacerbation of symptoms with posture versus exertion
- Most people with symptomatic LSS have limited walking capacity; they may require walking aids and may even avoid walking altogether
- Balance impairment, neuromuscular deficits in the lower extremities including decreased strength (weakness), sensory deficits (numbness), and absent or decreased reflexes (Achilles tendon and patellar)
- MRI is best, gives good soft tissue detail, but review found it is similar to CT for the diagnosis of lumbar spinal canal stenosis
- anteroposterior diameter (<10 mm) and cross sectional area (<70 mm2) of the spinal canal
- Non-pharmacological
- Physiotherapy related treatments include - balance training, specific exercise in lumbar flexion, lumber semi-rigid orthosis, braces and corsets
- Pharmacological
- Simple analgesia
- NSAIDS equivalent to paracetamol
- opioids may be used
- low quality evidence for use of vitamin B1 and gabapentin
- Injections
- meta-analysis published in 2015 found that epidural steroid injections provide limited short term and long term improvement in pain and walking distance in patients with LSS
- Surgical
- often an elective procedure
- decompression surgery for neurovascular structures
- other procedures also exist, see review BMJ 2016;352:h6234
Crystal arthropathy
Crystals found in synovial fluid
Calcium Pyrophosphate Dihydrate Arthropathy
- Monosodium urate monohydrate = acute gout, tophaceous gout
- Calcium pyrophosphate dehydrate = spectrum, acute pseudogout, destructive arthropathy, asymptomatic
- Basic calcium phosphate = Milwaukee shoulder
- Calcium oxalate = acute arthritis
- Lipid = acute arthritis
- Patients with an acute attack can often pinpoint the onset to the hour. They may describe the pain as the most severe they have ever experienced.
- Morning stiffness is prominent and reflects the underlying inflammatory mechanism
- Fevers, chills, malaise
- Most commonly involved are joints in the feet, especially the first metatarsophalangeal, tarsometatarsal, and ankle joints
- Pattern is usually monoarticular or oligoarticular (<4 joints). Can be polyarticular, affecting multiple joints in the hands and feet, especially in older people.
- Presence of family members with gout at a fairly young age may suggest a genetic defect in a specific enzyme
- Acute gout natural Hx favours self termination in majority, because blood and oedema increase pH, increase temp, decreases crystal formation; monoarticular mainly. This leads to an intercritical period for weeks/ months [ongoing damage can occur] --> complicated gout with longer duration, polyarticular in features and chronic tophaceous destructive gout [transitions to this when inter-critical periods no longer pain free
- Increased production (10%)/ intake vs decreased clearance (90%)
- Production: genetic due to PrPP synthetase mutation, acquired due to myeloprolif, high intake, alcohol, obesity, high trigs. 1/3 from diet, 2/3 endogenous
- Urate produced from purines (dietary = red meat, seafood, bacon, dairy and coffee protective, alcohol = beer>wine>spirits, endogenous)
- oestrogen reduces hyperuricaemia therefore less incidence in females cf males
- transplant (tacro and cyclosporine are risk factors)
- Reduced Excretion 90%: genetic due to HRPT mutation, renal disease, HTN, drugs (ASA, diuretics, cyclosporine, thiazides, frusemide)
- Urate excreted from kidneys
- Based on aspirate showing negative bifringement crystals that are rod and needle shaped
- CPPD crystals are weakly positive bifringement, rhomboid shape
- Radiology: Soft tissue swelling, eccentric opacities, punched out erosions with sclerotic margins and overhanging edges. Can use dual energy CT to differentiate CPPD from urate, best utilised for inaccessible joints
- Non-pharmacological: Rest, ice, compression, elevation
- Pharmacological Mx of acute gout:
- NSAIDs: need dose upper limit of normal, normal CIs for NSAIDS exist
- Colchicine: disrupts microtubule fx --> low dose = high dose with less SE, use in acute situation, long term SE = neuromyopathy in renal impairment
- Systemic corticosteroid = need 30 – 50mg for 5d, other option = depot ACTH (40mg IM)
- Intra-articular corticosteroid = req technical competence, skin atrophy at site of inj, rapid onset of action, well tolerated
- Canakinumab (IL-1b) in an RCT, good evidence coming, licensed in EU
- Anakinra: IL-1R antagonist, shorter half life than canakinumab
- Pharmacological Mx of chronic tophaceous gout
- Symptom control/suppression – colchicine can be used 0.5mg daily
- EMG/ NCS mild axonopathy, myoneuropathy risk,
- low dose oral corticosteroids, evidence for IL-1 inhibition (anakinra, canakinumab) in trials.
- Reduce urate load, aim <0.36mM (treat to target):
- Indication for Rx with hyperuricaemia + gouty arthritis (tophi, erosions, >2 attacks/yr, urate nephropathy, urate calculi), NOT Rx if asymptomatic and non of the aforementioned as toxicity too great and evidence of benefit lacking
- Allopurinol inhibits xanthine oxidase, start low, dose 100 – 800mg. NOT TO BE USED WITH AZATHIOPRINE, renally excreted, risk of hypersensitivity [HLAB5801, occurs <6w into dose significant --> DRESS (Drug rash with eosinophilia and systemic symptoms + interstitial nephritis + hepatitis)
- Feboxistat, now licensed, non purine analogue inhibitor of xanthine oxidase --> allopurinol allergy pts
- Uricosouric agents --> effectively inhibit uric acid reabsorption in prox tubule [URAT1/ OAT4 inhibition] eg probenecid + losartan
- Symptom control/suppression – colchicine can be used 0.5mg daily
Calcium Pyrophosphate Dihydrate Arthropathy
- Risk factors: Age, female, metabolic [hypophosphataemia, hypomagnesaemia, hyperparathyroidism, OA, haemochromatosis, wilsons disease]
- Presentation: There are a number of different presentations listed below (courtesy of BMJ best practice)
- An acute, typically mono-articular inflammatory arthritis often affecting large joints such as the knee
- A polyarticular inflammatory arthritis affecting large and small joints
- A chronic polyarticular arthritis, characterised by superimposed acute attacks of inflammatory arthritis.
- Osteoarthritis and CPPD without an inflammatory component
- The chronic form of CPP arthritis mimics osteoarthritis or rheumatoid arthritis and is associated with variable degrees of inflammation
- Dx: Effusion --> positive bifringement crystals (weakly), rhomboid shape, may miss
- Radiology = chondrocalcinosis, esp meniscus
- Rx: Joint aspirate, immobilization, NSAIDS, intra-articular and systemic steroids
Rheumatoid Arthritis
History
- Natural Hx: 5 – 20% self-limiting polyarthritis; 5-20% minimally progressive disease, 60 – 90% progressive disease
- Palindromic rheumatism, sudden onset, peaks within hours, usually large joints, no structural damage, important to recognise b/c Rx with hydroxychloroquine
- Morning stiffness (ask if >60min)
- All peripheral joints and cervical spine can potentially be affected
- DIP joints NOT affected
- Flexor and extensor tenosynovitis of hands
- Tendon rupture (usually extensor)
- Atlanto-axial instability in severe RA
- Fatigue and weight loss
- Extra articular symptoms include the following
- Eyes: Sicca symptoms, scleritis, corneal ulcers
- Skin: Ischaemic ulcers and digital gangrene, Rheumatoid nodules in Pts who are RF +ve
- Lungs: Pleural effusions, nodules and ILD
- Nerves: Compressive neuropathy (carpel tunnel), Mononeuritis multiplex
- Lymphoma (B cell) 2-3 fold increase
- Capillaritis
- Felty's syndrome, triad of:(1) Neutropenia (2) Splenomegaly and (3) Deforming RA
- For detail see Rheumatology short case section
- General inspection:
- Cushingoid
- Rheum: Symmetrical deforming polyarthropathy of the small and large joints
- Skin: Rheumatoid nodules, evidence of capillaritis
- Lungs: effusions and fibrosis
- Cardiac: pericardial rub
- Abdomen: splenomegaly of Felty’s, Epigastric tenderness from ulcer/gastritis d/t prednisone or NSAIDs
- Eyes: sicca, episcleritis, scleritis
- FBC: Anaemia of chronic disease
- UEC: decreased renal function with secondary amyloidosis, order urine albumin: creatinine ratio to help quantify
- CRP + ESR: Raised inflammatory markers
- CXR: Pleural effusions (exudative) in 5% of Pts, low pH, very low glucose and RF+
- Joint aspirate: Inflammatory fluid: WC 200 - 2000
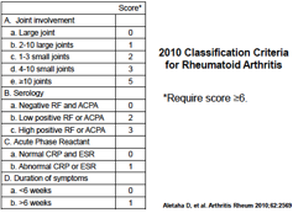
- Serology: RF positive in 70% of pts, predicts severe joint disease and increased likelihood of extra-articular features, Anti-CCP: similar sensitivity but greater specificity, adverse prognostic factor
- Radiological features: (1) periarticular soft tissue swelling (2) deformities (3) joint subluxation (4) juxta-articular osteopenia (5) periarticular erosions (6) symmetrical joint space narrowing
- MRI findings: looking for 3 things: synovitis, marrow oedema in bones surrounding inflamed joints (best predictor of development of erosions), erosions
- Goals: (1) Confirm Dx (2) Optimise symptoms (3) Prevent deterioration/ progression
- Simultaneous control of symptoms and retard progression of erosive disease, frequent monitoring to determine lack or progression of disease
- Symptom control:
- NSAIDS/ stronger analgesia/ corticosteroids/ local injection of corticosteroids
- Retard progression: achieve remission [DMARDS = biological vs non-biological or traditional]
- DMARDS: indicated if (1) New presentation AND active disease, start within 3/12 (2) seropositive disease (3) erosions on X-ray (4) clinical deformities
- bDMARDS --> no remission despite 6/12 trial DMARDS
- DMARDS improve cardiovascular mortality
- Mild disease [defined by <6 joints + RF neg + non-erosive]
- NSAIDS, if active then hydroxychloroquine [SE = visual field defects, scotomoas, colour blindness]/ sulfasalazine [SE = rash, gastrointestinal, aplastic anaemia, hepatitis – monitor LFTs frequently]
- hydroxychloroquine requires yearly ophthalmologic reviews
- Severe disease [> 6 joints, active synovitis, erosions, RF +, high ESR/CRP]
- NSAID + Pred [bridge Rx until DMARDS take effect, slows radiology progression, decreases synovitis], + MTx [contraindicated in hepatic – 1/100 severe fibrosis Aus study 1994, renal, lung disease – bilateral alveolar infiltrates, hypoxia, decr DLCO, Rx pneumonitis --> pred 60mg 2-4/52 noting majority recover completely; those who can’t stop EtOH, LFTs monitored 1-3/12, use folic acid, risk of lymphomas --> reverses when ceased MTX]
- If no response, increase MTX dose OR add 1 off [sulfasalazine/ hydroxychloroquine/ leflunomide --> inhibits DHODH which is needed for de-novo pyrimidine synthesis, activated T lymphocytes don’t have salvage pathway!, very long t/12 b/c enterohepatic re-circulation need cholestyramine washout, diarrhea (30%), peripheral neuropathy and ILD rare s/e/; NOT FOR use in pregnancy, cyclosporine]
- Biologics
- TNF-alpha --> [preRx screen for HBV/HCV/HIV/TB vaccinate pneumococcus + flu, No live vaccines 3 weeks before and up to 3 months after, Auto-abs esp for infliximab 40%, reason for Rx failure, give with MTX reduce prevelance of Abs, cases of demyelination syndrome exist, cancers = skin, small risk lymphomas]
- If Mantoux/ IGRA + --> pretreat for 2/12 INZ then continue Rx for 9/12, TB usually presents with extra-pulmonary disease
- Abatercept = CTLA4 bound to Ig, inhibitory co-stimulation to T cells. Give in combo with MTX, non inferior to TNFs, less infection risk esp in bronchiectasis
- Tocilizumab = IL6R mab, prevents signaling down IL-6-IL-6R signal transduction, NO NEED FOR MTX, and only bDMARD monoRx > MTX monoRx, only biological agent approved for single use, > adalimumab in efficacy. SE = ALT/AST up, dyslipidaemia, opportunistic infections, bowel perf! --> contraindicated if have diverticulitis
- Rituximab: Use only if RF+/ ACPA+, effective if MTX resistant + TNF-alpha failed, use if have infection or malignancy
- Tofacitinib: small molecule inhibitor [works intracellularly] of janus-kinase-STAT pathway activation (JAK3,1 >2), PBS for monotherapy or combo with MTX, SE similar to tocilixumab
- TNF-alpha --> [preRx screen for HBV/HCV/HIV/TB vaccinate pneumococcus + flu, No live vaccines 3 weeks before and up to 3 months after, Auto-abs esp for infliximab 40%, reason for Rx failure, give with MTX reduce prevelance of Abs, cases of demyelination syndrome exist, cancers = skin, small risk lymphomas]
- Treatment Algorithm: Dx then start NSAID + Prednisolone + MTX [leflunomide if MTX contraindicated] --> if no response 6/12 then biological or other DMARDS b vs non-b [decision based on poor prognosis markers such as RF+, ACPA+, erosions, high disease activity]
- Pregnancy --> contraindicated are MTX, leflunomide, cyclosporine, cyclophosphamide + NSAIDS [PDA closure], can use hydroxychloroquine, sulfasalazine, azathioprine
- Aggressively manage cardio-metabolic risk factors as chronic disease is associated with accelerated atherosclerosis
SLE
General factoids
- Female: male 10:1, decreases post menopause to 1:1, onset 15-40yo
- Survival --> worst for hispanics, but even then 5yr = 87%
- Etiology: Multifactorial and polygenic (STAT4, PTPN22), Complement defeciency (C1q = 90% chance of developing lupus!, C4), environ (smokers, UV, EBV), hormonal (VitD)
- ACR criterion for Dx and other clinical features
- Req 4 with 1 clinical [acute/ subacute/ chronic cutaneous lupus, oral ulcers, non-scarring alopecia, synovitis, serositis [pleural>pericardial, common problem!], renal = 500mg proteinuria or RBC casts, neurologic manifestations, anemia, leukopenia, thrombocytopenia] and 1 immunological [ANA (+ 95-99%), dsDNA (best for monitoring disease activity), DAT+, anti-Sm (most specific, remain + even in remission, assoc with renal and CNS disease), anti-ribosomal P10 (in Asia), phospholipid +, low complement]. Other immunology = SSA (neonatal lupus, congenital heart block, cutaneous) > U1RNP (myositis, raynauds) > SSB (neonatal lupus, cutaneous), CRP does not correlate with disease titre.
- Can Dx lupus if renal Bx proven without above criterion
- Protean manifestations with myalgia, malaise, fevers
- Skin: can have ANA neg lupus as Ro-52 antigen not eluted with ANA, annular rash with central clearing = classic Ro-associated subacute cutaneous lupus
- Arthritis/ arthralgia = most common clinical presentation, even nodules can happen, non –erosive but deforming, correctible = jacoud’s arthropathy
- Lung involvement: pneumonitis, serositis, shrinking lung [diaphragmatic dysfx + pulm fibrosis], PE, pulmonary hypertension [ACA], pulmonary haemorrhage.
- Heart: serositis, conduction block, liebmann-sacs vegetation [50% autopsy, assoc with ApL]
- Accelerated atherosclerosis: 2-5x death, accelerated by prednisolone, statins for LDL >3, BP >130 --> ACE/ARB
- Renal disease: worst prognosis, symptomatic only in advanced disease, need regular monitoring, bx if increasing creatinine with nil other cause OR proteinuria 1g OR protein 500mg + >5RBC/HPU OR protein 500mg + cellular cast
- Class 1: minimal mesangial = normal LM, no Rx, ACE for proteinuria
- Class 2: mesangioproliferative, no Rx, ACE
- Class 3: focal prolif <50% Glomeruli, Rx indicated
- Class 4: diffuse prolif >50% glomeruli, Rx indicated
- Class 5: membranous, Rx if in nephrotic range
- Class 6: advanced sclerosed --> >90% glomeruli sclerosed, no Rx, burnt out
- Neurological: 5 commonest syndromes (1) headache (2) mood disorder (3) sz (4) cognitive dysfx = most common (5) cerebrovascular disease, MRI most useful [atrophy = commonest finding, look for increased signal intensity both white + grey matter], assoc with APL + anti-ribosomal P10
- Antiphospholipid syndrome: [prior pregnancy loss OR prior thrombosis AND mod high titre of aCL, LAC , B2GP1 done 12/52 apart], primary or secondary [10-30% lupus pts], LAC = pregnancy worse, triple positive = lots of thrombosis
- Neonatal lupus: Congenital heart block develops in 2-3% of mothers with SSA/SSB, 60% req pacemaker, 20% die; cutaneous lupus will clear by 6/12
- Assess for steroid use: Cushingoid or prox myopathy
- Rheum for Symmetrical, deforming polyarthropathy - reducible
- Skin for alopecia or Rash
- Lungs for fibrosis or effusion
- Heart for pericarditis, murmur for liebmann-sacs endocarditis
- Abdo for hepatosplenomegaly
- FBC: chronic anaemia, macrocytocis if MTX is used, DAT for evidence of haemolytic anaemia
- UEC: raised creatinine, urinalysis, casts, microscopy for casts, glomerular red cells, proteinuria
- C3/ C4 levels - active disease associated with complement consumption. Also complement deficiency adverse prognostic marker
- CRP: not correlated with disease activity but if elevated means that the inflammation is arising from somewhere else
- ESR
- ANA: elevated in >95% of SLE, can have ANA negative lupus in chronic cutaneous lupus with Ro-52+, ENA +, dsDNA (correlates with disease titre), anti-Sm more specific, not correlated with disease titre, anti-phospholipid antibodies, U1-RNP associated with mixed connective tissue disease
- Renal biopsy
- Imaging of joints for arthropathy
- Goals: Confirm Diagnosis, Optimise Symptoms, Prevent Deterioration, Manage Exacerbations
- Symptom managment
- NSAIDS for arthralgia, synovitis, constitutional symptoms
- Avoid sun exposure/ use sunscreens
- Stop smoking
- All patients should be on hydroxychloroquine
- S/E = maculopathy after prolonged use, more common in renal dysfx, irrerversible if get bull’s eye maculopathy, screening at baseline then annual opthal assessment
- Corticosteroids: initial control for inflammation
- MTX --> arthritis, skin rash, constitutional sx
- Leflunomide --> arthritis, or if methotrexate is contra-indicated
- cyclophosphamide --> major organ involvement
- Renal: Treat 3,4, 5 agressively.
- Class 3 & 4 induction: MMF for 6/12 [Hispanics/ afro-americans] OR cyclophosphamide [500mg 2nd weekly x 6 esp whites] AND Pred [1g x 3 pulse then taper 0.5-1mg/kg/d]; Maintainence [AZA or MMF]
- Class V --> Rx if nephrotic [>3g/d] with MMF + Pred, no improvement in 6/12 --> cyclo
- Neuropsychiatric lupus: Cyclophosphamide + corticosteroids
- APLS --> thrombosis = INR 2-3 indefinitely, if thrombosis on warfarin then INR 3-4 OR INR 2-3 + aspirin, no evidence for NOACS yet, no role for immunosuppressant, in pregnancy use aspirin + LMWH
- Pregnancy --> no active disease then monitor, mild disease --> hydroxychloroquine, severe disease --> pred, lupus nephritis --> pred/ AZA if necessary.
- Note mycophenylate can not be used in pregnancy, but if planning to be pregnant mycophenylate as induction better than cyclophosphamide
- Advice patient to take prophylactic pregnancy preventative measures if active disease
- Note that 60% relapse when pregnant
- Risks of worsening renal function
- Risk of neonatal lupus
- Rituximab --> Rx resistant disease; seems to be race related [better in afros and Hispanics]
- Belimumab --> blocks BLyS [survival cytokine upregulated in active lupus], evidence accumulating
Seronegative spondyloarthropathies
Ankylosing spondylitis
Epidemiology and general factoids
Psoriatic arthropathy
Clinical Features
Epidemiology and general factoids
- Inflammatory arthritis of the axial skeleton with extra axial and extra articular involvement
- Progressive stiffening and fusion of the spine
- Strong association with the HLA B27 gene, 90 - 95%, 0.5 - 1% pop suffer from AS, male: female 3:1, 5% of population have HLA B27
- Often there is a 9 yr delay to diagnosis
- Inflammatory back pain:
- Insidious onset
- improvement with exercise
- No improvement with rest
- Nocturnal pain that improves on walking
- (Responds to NSAIDs)
- Buttock pain – often alternating, poorly localized (sacro-ilitis)
- Restriction in spinal movement
- Characteristic posture
- All segments of spine have reduce movement
- Chest expansion reduced (costo-vertebral joints)
- Final stage of AS with severe kyphosis of thoracic and cervical spine
- Straightening of cervical lordosis
- Exaggeration of thoracic kyphosis
- Straightening of lumbar lordosis
- Hip involvement as well in this patient: Fixed flexion deformity of both hips
- Extra-articular manifestations
- anterior uveitis - painful red eye, photophobia, blurred vision, with recurrence a problem. Can be a HLA B27 associated disease without ankylosing spondylitis
- Inflammatory bowel disease - 70% have microscopic subclinical asymptomatic colitis
- Osteopenia
- Cauda-equina, cervical myelopathy
- Fractures
- Cardiac: CVD risk, aortic regurgitation, conduction disturbance, accelerated atherosclerosis
- Respiratory: chest wall restriction, apical fibrosis (apical fibrosis is usually asymptomatic, chest wall restriction is more common cause of symptoms)
- Secondary amyloidosis
- Image SI Joints: If sacroilitis present then it significantly increases the likelihood of spondyloarthritis
- Early changes: erosions, sclerosis at joint margins
- Later: pseudo-widening of joint (combination of erosions)
- Last: joint space narrowing progressing to ankylosis
- Need to demonstrate Sacroilitis to obtain Rx with biological agents
- Cervical and thorac-lumbar spine:
- Vertebral squaring: due to erosion at corners of the vertebral bodies (where annulus fibrosis attaches) -> this can develop into a Romanus lesion with sclerosis of the bone (compare to one above)
- Syndesmophyte
- MRI in spondyloarthritis: Bone marrow oedema, erosions are detected earlier
- Physiotherapy/exercise program and NSAID
- May be effective in preventing radiographic progression
- Need to have had trial of physiotherapy and NSAIDS to escalate to biological agents (trial for 3 months)
- Axial disease
- After NSAID/Exercise -> next step is TNF blockers (no evidence for other disease modifying drugs)
- Local corticosteroids can be useful for sacro-iliac disease or troublesome facet disease
- Peripheral disease
- Sulfasalazine for peripheral arthritis (but no evidence for other disease modifying agents)
- Local corticosteroids can be useful
- TNF inhibitors (infliximab/etanercept/adalimumab): 70-90% get improvement in symptoms
- TNF inhibitors
- Previously thought that despite being fantastic for symptoms did not affect radiographic progression
- Recent prospective longitudinal study in 330 patients found
- TNF inhibitor use was associated with less radiographic progression
- Early initiation and longer duration of tratment seemed more protective
Psoriatic arthropathy
Clinical Features
- 5 distinct patterns of arthritis
- Asymmetric oligoarthritis/monoarthritis
- Polyarthritis – symmetric
- Spondylo-arthritis – axial, AS like
- Distal interphalangeal joint with nail disease
- Arthritis mutilans
- Skin disease
- Dactylitis – ‘sausage digit’
- Enthesitis
- Nail changes more common
- Classic radiological involvement: juxta-articular involvement, pencil in cup deformity
- Physiotherapy, multi-modal analgesia, NSAIDS
- Avoid systemic steroids because rapid wean of topical steroids can cause flare of skin disease
- DMARDS (methotrexate, sulfasalazine and lefluoamide) used for peripheral disease
- Biological agents are anti-TNF agents
Systemic Sclerosis
Epidemiology of scleroderma:
- Rare disease, female > male, age of onset 40 – 60, limited > diffuse, environmental toxins implicated
- FHx strongest RF, but still very small
- Arthralgia 98% reported [erosive in 25%]
- Legs: ulceration, vasculitis
- Tenosynovitis with tendon friction rub --> worse prognosis
- Myalgia --> may have biopsy fibrosis secondary to disease
- GIT --> eosophageal hypomotility, GAVE, poor prognostic indicator
- Lung disease:
- ILD, lung fibrosis is cause of death usually
- DLCO<50 assoc with worse prognosis and assoc with pulm HTN, progression occurs early in on the course of the disease [first 5y], Scl70 predictor of getting disease, anti-centromere protective
- Histology = NSIP (90%)> UIP [worse] pattern, in fact HRCT is the most powerful predictor of mortality
- Dx --> HRCT, DLCO, 6 min walk test
- Rx --> cyclophosphamide for 12/12, BMTx trials St Vincents, RPAH
- Cardiac disease
- fibrosis, conduction deficits, coronary spasm, assoc with diffuse disease + Scl-70, effusions in 30 – 40%
- Renal disease:
- hypertensive crisis, secondary to microvacular changes, assoc with RNA polymerase antibodies, renal crisis assoc with HTN + oliguric renal failure, use ACE-inhibitors
- Scleroderma classification
- Localised – morphea
- Limited scleroderma: long Hx raynauds, scleroderma distal to knees and elbows, anywhere else = diffuse, lung disease --> pulmonary HTN + digital ischaemia > ILD, cardiac and renal disease rare, Antibodies = centromere, nucleolar and speckled, if centromere + --> decreased risk of ILD + pulm HTN
- CREST syndrome
- Diffuse scleroderma: recent onset raynauds, skin disease rapid, renal and cardiac involvement, lung disease ILD > Pulm HTN, antibodies Scl70 (predict lung) and RNA polymerase (1 in 8 will have renal crisis)
- Skin disease pattern --> rapid progression of skin change, plateu, skin soften and can go back to normal skin
- DDx eosinophilic fasciitis, here fingers are spared cf scleroderma, assoc with orange peel skin,
- Nailfold capillaroscopy --> dilated loops + areas of drop out consistent with scleroderma/ Dermatomyositis pattern
- Stem cell Tx --> case reports show complete resolution, disease progression 10%, most have 60-70% improvement
- Smokers no benefit from Rx, need careful screening as mortality mainly from cardiac causes
- Occurs in 12% of patients with both limited and diffuse disease
- Later complication: 5-10 years of duration of disease
- High mortality
- Dx
- Suspect in patients with DLCO < 50% and minimal fibrosis on HRCT --> ECHO
- ECHO: pulm pressure >50 --> right heart cath
- Mean pulmonary artery pressure > 25mmHg with PCWP < 18mmHg
- Mean PAP on exercise > 30mmHg with wedge < 18mmHg
- Rx
- Warfarin
- Mainstay now is combination therapy include endothelin antagonists, PDE5 inhibitors and prostaglandins but single agent therapy only subsidized in Australia, and must show clinical stability in 6/12 for ongoing Rx
- Ambrisentan + tadalafil cf monotherapy reduced Rx failure by 50% in particular hospitalisations
- Rx only subsidized for WHO functional class III or IV
- Keep warm
- Dont smoke
- Topical nitrates
- Calcium channel blockers
- prostacyclin infusions if severe
- digital sympathetctomy if severe
- Physiotherapy
- Some evidence for stem cell transplant and cyclophoshomide.
- For diffuse skin thickening MMF/ MTX. Evidence for MTX in particular for early skin involvement from obesrvational studies therefore the evidence is relatively weak. Evidence for mycophenolate even weaker with small observational studies supporting its use.
- IVIG/ rituximab may be trialled in refractory cases
- Facial thickening and decreasing diameter of oral apeture - exercises
- oesophageal hypomotility management aims at diminishing risks of gastrointestinal reflux disease, managing strictures
- consideration for prokinetic agents such as metoclopramide
- small bowel bacterial overgrowth Rx with oral antibiotics
- pancreatic insufficiency --> Rx with pancreatic enzyme replacement
- Physiotherapy to limit joint immobility
- Simple NSAID based analgesia
- if inflammatory - consider glucocorticoids
- add hydroxychloroquine 200 - 400mg daily
- If not controlled consider methotrexate
- Pericarditis - normal management as per guidelines (colchicine + high dose NSAIDS)
- may develop cardiac tamponade physiology quickly - and with no chest pain
- Heart failure associated with reduced systolic ejection fraction is treated with standard heart failure treatments, such as angiotensin-converting enzyme (ACE) inhibitors, implantable-cardioverter defibrillators (ICDs), and cardiac resynchronization therapy (CRT
- While there are no established treatment practices for myocarditis associated with SSc, immunosuppressive agents are typically used in a manner comparable to that for the treatment of interstitial lung disease associated with SSc.