Ischaemic Heart Disease
This is usually part of a list of medical problems (either active or inactive) that the patient has, rather than the primary problem
Presentation
Presentation
- Typical angina symptoms (central crushing chest pain radiating to arms, shoulder, neck, jaw), worse on activity, relieved by rest - may be sudden onset and long lasting (>20m) if unstable, or crescendo angina (more frequent, longer lasting episodes)
- Determine when the symptoms came - how long ago was diagnosis made
- ECG (ischaemic changes - STEMI, TWI, ST depression, whelan's sign, LBBB), CXR (signs of LV failure, DDx infective process, pneumothorax), Bloods (esp troponin, CK-MB), ECHO (regional wall motion abnormality, dilated RV in PE, aortic flap in dissection)
- Exercise stress test (ECG, ECHO), pharmacological stress test (dobutamine induced), Cardiac catheterisation
- Cardiovascular risk equivalents --> T2DM, CKD
- Others: modifiable risk factors [smoking, obesity, dyslipidaemia, physical inactivity, diabetes, hypertension], non modifiable [age, gender, family history]
- Non-traditional risk factors: high sensitivity CRP, homocysteine, lipoprotein A, carotid intimal thickness, ABPI, coronary artery calcium score
- No driving requirements - no driving for 2 weeks post MI, no driving after ventricular arrhythmia, no driving for 2 days after stent placement
- Acute coronary syndrome patients should have early risk stratification according to well defined scoring algorithms such as GRACE, CRUSADE or TIMI
- Non-pharmacological: mainly lifestyle modifications --> diet, exercise, smoking, glycaemic control
- Diet --> DASH diet, mediterranean diet
- Smoking cessation - risk of recurrent infarction fell by 50 percent within one year of smoking cessation and normalized to that of nonsmokers within two years
- Cardiac rehabilitation - Multifactorial cardiac rehabilitation, which includes efforts to address all of the above issues, can produce significant long-term reductions in both total and cardiovascular mortality
- Pharmacological and invasive
- Stable coronary artery disease
- All patients should receive aspirin --> improves prognosis in meta-analysis, but don't do it if patient is on oral anticoagulation for atrial fibrillation as it increases bleeding risk without any benefit CIRCULATIONAHA.113.004834
- PTCA vs medical therapy: Improved outcomes if FFR guided PTCA used compared to angiographically guided PTCA
- Courage trial: decreases angina but does not improve outcome
- CABG compared to medical therapy improves outcome in (a) left main disease (b) 2 or 3 vessel CAD with proximal LAD and (3) 3 vessel CAD and impaired LVF
- CABG compared to PTCA:
- Same survival
- Increased procedures with PTCA
- Worse outcome in DM with PTCA
- Management of angina
- Treating episode of angina use GTN spray or GTN tablet
- Preventing further episodes of angina: Decrease myocardial oxygen demand by beta-blocker therapy (can use non-dihydro Ca channel blockers if contra-indication to beta blockers exist), increase myocardial oxygen supply (long acting nitrates, either a topical patch starting at 5mg/ 24 hrs applied for maximum 14h a day to give a nitrate free period or isosorbide mononitrate 30mg starting dose daily)
- Additional therapy to beta-blocker includes dihydro Calcium channel blockers such as amlodipine
- Ivabradine 5mg BD, if patient intolerant to Ca channel blockers or Beta blockers and in sinus rhythm
- Management of acute coronary syndrome:
- Fulfils STEMI criterion within time frame for immediate revascularisation (thrombolysis versus PCI)
- PCI preferred if given within 2hrs compared to thrombolysis in terms of short term mortality
- Symptoms onset < 1 hour – only accept PCI if available within 60 minutes (only accept shorter duration as this is the ‘golden’ hour). Otherwise thrombolyse and transfer to PCI capable hospital
- Symptom onset 1-3 hours – PCI within 90 minutes or thrombolyse
- Symptom onset 3-12 hours – PCI within 2 hours or thrombolyse
- If thrombolysed successfully then transfer to PCI centre within 3 - 24hrs, known as pharmaco-invasive approach, leads to reduction in recurrent ischaemic events.
- If thrombolysed unsuccessfully, then transfer to PCI centre for immediate rescue angioplasty
- Aspirin is important, addition of clopidogrel reduces risk of recurrent MI
- Prasugrel > clopidogrel in terms of in-stent thrombosis reduction, but increased risk of bleeding in some patients – previous stroke/TIA, age > 75 and weight < 60kg
- Ticagrelor vs clopidogrel - primary end point (a composite of death from vascular causes, myocardial infarction, or stroke) occured less with ticagrelor at the expense of greater non-procedural (non-CABG related) bleeding
- Anticoagulation therapy - heparin vs LMWH - Grade 1 suggestion that all patients with ACS should have anti-coagulation therapy. If planning an early procedure then UFH, if conservative then LMWH
- ACE-inhibitor --> HOPE trial showed that ramipril – reduced risk of CV death, MI or stroke even in patients who are not hypertensive post ACS
- Statin --> High dose statin has proven evidence in reducing the combined end-point of CV death, MI or stroke
- Beta-blockers should be used, continue for up to three years post myocardial infarction (although evidence for this is not robust), aiming HR < 70
- Eplerenone (mineralocorticoid receptor antagonist) in patients who have had LV failure (<40%) post AMI
- Stents
- DES elutes an anti-proliferative drug which decreases the re-stenosis rate however at the expense of higher late stent thrombosis rates due to decrease in epithelialisation.
- Requires 12 months of dual antiplatelet therapy.
- Recommended if having long lesion in small vessel, restenosis or diabetes
- should avoid if surgery indicated within 6 months
- BMS have increased rates of in-stent restenosis but decreased late-stent thrombosis
- dual antiplatelet agents recommended for 6 weeks (eTG)
- DES elutes an anti-proliferative drug which decreases the re-stenosis rate however at the expense of higher late stent thrombosis rates due to decrease in epithelialisation.
- Fulfils STEMI criterion within time frame for immediate revascularisation (thrombolysis versus PCI)
- Stable coronary artery disease
- Surgical management
- Depending on anatomy and co-morbidites, eg left main disease, multi-vessel disease, significant LV dysfunction, other anatomical difficulties. Scoring systems aid this - eg syntax score
- LIMA to LAD may be done off-pump (on a beating heart), LIMA has greater long term graft patency than RIMA or a Radial artery graft
- Radial artery may be utilised, as can the saphenous vein.
- There is no difference in stroke rate with off-pump bypass c/f with on-pump (NEJM 2012)
- Over 10 years, in patients with ischaemic cardiomyopathy (EF <35%) who had CAD amenable to CABG, there was improved survival in patients who had CABG + medical therapy compared to medical therapy alone. NEJM 2016 - STICH extension study.
- LV failure
- Surgical revascularisation vs heart failure drugs vs transplant
- Arrhythmia
- AICD, esp 30 days post AMI
- VSD, Acute MR
- Look for median sternotomy scar and the harvest scars (radial artery, saphenous vein). Saphenous vein harvesting scar breakdown is far more common than sternal wound breakdown
Infective Endocarditis
Patients may be found in the in-patient setting or the out-patient setting with IV pump infusions.
Presentation
Presentation
- Malaise, fevers, chills, rigors, symptoms of anaemia, haematuria (glomerulonephritis secondary to deposition of immune complexes)
- Acute onset (suggests S. aureus) vs subacute onset - weeks to months, presents with PUO
- Symptoms of embolic events (splenic infarcts, rapidly appearing rash, stroke syndrome)
- Symptoms of congestive cardiac failure, syncope secondary to progressive AV block
- How diagnosed? Blood cultures should have been taken, serology for culture negative, Echocardiographic confirmation. Remember modified DUKES criterion and the presence of major and minor features
- Major features include (1) confirmed bacteraemia with typical organisms on 2x BC (2) persistent BC with unusual organisms (3) Endocardial involvement as demonstrated by ECHO evidence --> oscillating mass, abscess, new partial dehiscence of prosthetic valve (3) New regurgitant murmur (4) Positive culture for C. burnetti
- Minor features include (1) immunological features such as glomerulonephritis (2) embolic features such as stroke, splenic infarcts, splinter haemorrhages (3) fever > 38 (4) Predisposition such as rheumatic heart disease, prosthetic valves, unrepaired congenital heart disease, IVDU (5) Suggestive microbiology
- To diagnose require 2 major, 1 major 3 minor, 5 minor
- Ask about the number of blood cultures that were positive - noting that persistently positive blood cultures is in and of itself an indication for cardiac surgery - Persisting fever and bacteraemia > 7-10 days
- Consumption of classical pathway complement proteins C3, C4
- History of dental procedures, poor oral hygeine, infected intravenous access devices
- Past history of rheumatic fever secondary to GAS infection (ask about migratory arthritis, heart failure, sydenham's chorea)
- Prosthetic valves, other heart operations, congenital heart disease eg bicuspid aortic valve, repaired tetralogy of fallot's
- IVDU is particularly associated with right sided endocarditis
- Immunosupression - steroid use etc
- If S. bovis, ask about colonoscopy
- Empirical therapy - IV antibiotics initially with gentamicin + benzypenicillin + flucloxacillin, if MRSA suspected replace fluclox with vancomycin
- Gentamicin only used for synergistic effect for streptococcal and enterococcal species, start empirically
- Generally treatment is given for 2 - 6 weeks intravenously
- prosthetic valve infections - vancomycin is added in the regime, rifampicin may also be used (or moxifloxacin) in order to penetrate the biofilm
- Involvement of a cardio-thoracic surgeon
- Indications for surgery:
- heart failure secondary to regurgitant/ obstructive lesion, fistulisation into chamber or pericardium
- Signs of uncontrollable infection - abscess, false aneurysm, persistent fevers and BC > 7 - 10d despite medical therapy, infection caused by fungi/ multi-resistant organism
- Prevention of embolic phenomenon - large (>10mm) or very large vegetations (>15mm)
- Prophylaxis: antibiotics indicated only for (1) patients with prior episodes of infective endocarditis (2) patients with prosthetic heart valves (3) congenital heat malformation, either unrepaired cyanotic heart disease or repaired cyanotic heart disease with residual defects. Prophylactic regimens include high risk procedures such as dental or oral surgery - amoxicillin 2g 1 hr prior to the procedure, no need to give prophylaxis for gastrointestinal or genitourinary procedures
- Embolic phenomenon - mycotic aneurysms, splenic infarcts, strokes
- Heart failure
- AV block secondary to peri-annular extension of infection - requires source control for cure, may require pacemaker
- Splenic abscess - may have persisting fevers
- Immunological phenomenon - glomerulonephritis
- Hands - clubbing, splinter haemorrhages, oslers nodes [painful], janeway lesions [not painful]
- Eyes - Roth spots, conjunctival petechiae
- Abdomen - splenomegaly
- Urinalysis - haematuria for GN
- Heart - MR > MS > AS > AR
Atrial Fibrillation
History
- palpitations, angina, dyspnoea, presyncope, fatigue
- complications of AF: stroke, TIA, mesenteric ischaemia, CCF
- CHADS2-VASC score - a calculation of the risk of systemic embolisation
- History of treatment, including warfarin, INR monitoring (doses and records), bleeding complications
- previous DC cardioversions, attempts at rhythm control
- drug interactions and side effects
- Irregularly irregular pulse
- signs of hyperthyroidism
- signs of CCF
- Anticoagulation
- Calculate CHADS2-VASC score
- All studies have concluded that the benefit from anticoagulation significantly exceeds the risks for almost all AF patients with a CHA2DS2-VASc score ≥2
- Choice includes pharmacological - warfarin, novel oral anticoagulation agents or non-pharmacological - left atrial appendage occlusion devices eg watchman's procedure
- Atrial appendage occlusion device is non-inferior to warfarin, 1-2% risk complication of implant, only if contra-indication to warfarin
- NOAC agents include apixaban, rivaroxaban, edoxaban and dabigatran
- Dabigatran [150mg BD or 110mg BD, 80% renally excreted, dialyzable drug, stop 48hr before Sx, if mod renal – 96h before], Rivaroxaban [10 – 20mg OD, non inferior, less ICH bleeding], apixaban BD dosing, similar to rivaroxaban but IMJ 2014 suggests can use up to CrCl >=25
- Less drug interactions than warfarin. Dabigatran interact with p-gp inhibitors [verapamil], rivaroxaban interaction with CYP3A4 [not as bad as warfarin]
- Dabigatrin --> most sensitive = Thrombin Time > APTT, confirm with haemaclot test [dilute thrombin clotting time], Rivaroxaban = PT, but does not estimate its effect, therefore can be grossly high without consequence, consider drug specific Xa level!, apixaban = factor-Xa levels
- In periop stopping drug prior to Sx --> driven by half life [3 if low bleeding, 5 if high bleeding, noting effect of renal fx on half life
- In general, there is a similar or lower risk of systemic embolisation with NOACS when compared to warfarin with decreased major bleeding risk, especially intracranial bleeding
- reversible agents are being developed and exist for dabigatran (idracuximab), rivaroxaban and apixaban (andexanet alfa)
- Dabigatran [150mg BD or 110mg BD, 80% renally excreted, dialyzable drug, stop 48hr before Sx, if mod renal – 96h before], Rivaroxaban [10 – 20mg OD, non inferior, less ICH bleeding], apixaban BD dosing, similar to rivaroxaban but IMJ 2014 suggests can use up to CrCl >=25
- there is no compelling evidence for the use of aspirin as monotherapy
- when initiating therapy bridging is not required for warfarin
- There is a lack of evidence to support the use of NOACS in valvular AF
- Calculate CHADS2-VASC score
- Rate control [better LVEF after rate control]
- If required rapidly --> IV verapamil or beta-blocker [5mg IV]
- lenient control non inferior to strict control (that is aim HR < 110 cf <80)
- beta-blockers, non-dihydropyridine calcium channel blockers, digoxin and amiodarone can be used as rate control in this setting
- if there is significant hypotension or advanced heart failure, digoxin should be first option
- If digoxin is used, digoxin levels should be obtained periodically
- Rhythm control
- Rhythm control [equivalent strategy to rate control in AFFIRM, only for those with persistent symptoms]
- flecanide if there is no structural heart disease, otherwise sotolol, amiodarone
- If AF occurred after 48 hours then patients should be anticoagulated for 3 weeks prior to cardioversion and 4 weeks unless TOW is performed beforehand
- DC cardioversion if unstable - need to synchronise shock, 200J
- Catheter ablation procedures
- pulmonary vein isolation - more successful than anti-arrythmics at maintaining SR
- AV node ablation + PPM
- atrial reduction surgery
Congestive Cardiac Failure
History
- Dyspnoea - quantify at what level of activity
- orthopnoea and paroxysmal nocturnal dyspnoea
- peripheral oedema
- weight gain
- symptoms of a specific cause - eg arthropathy of haemochromatosis, chest pain of myocardial ischaemia
- Causes of exacerbation
- non compliance with treatment, whether it be medications, fluid restriction or salt intake
- acute myocardial infarction
- arrhythmia, especially atrial fibrillation
- anaemia
- infection
- medications such as NSAIDS, steroids due to fluid retention
- thyrotoxicosis
- surgery
- pregnancy
- function at baseline in terms of NYHA class
- I = asymptomatic, II = dyspnoea with mod activity (climbing stairs), III = dyspnoea with mild activity (putting clothes on), IV = dyspnoea at rest
- Risk factors
- those predisposing to hypertension
- alcohol, viral illness, haemochromatosis
- medications such as trastuzumab, anthracyclines
- Investigations
- BNP has negative predictive value and some studies show that it correlates with prognosis
- TFT/ Fe studies
- CXR
- TTE
- Angiogram/ MIBI
- Endomyocardial biopsy
- Cardiac MRI
- Viral serology
- Serum ACE level, rectal fat pad biopsy
- Complications
- arrhythmias
- symptoms of left heart failure
- symptoms of right heart failure including congestive liver disease and ascites
- Thorough cardiovascular exam, looking for S3, S4, displaced apex beat, heaves, thrills, valvular pathology
- Comment on whether the patient is euvolemic or hypervolemic
- Examine for specific causes - eg angioid streaks in acromegaly, paget's disease in high output cardiac failure
- Presence of cardiac devices
- Non pharmacological measures
- Cardiac rehabilitation including multidisciplinary team that involves physiotherapist, occupational therapist, dietician
- this improves functional capacity, symptoms and neuro-humoral abnormalities
- reduces hospitalisations
- increases survival
- improves quality of life
- low calorie, low fat fiet, high fibre diet
- sarcopenia may be common - may need to investigate for malnutrition
- low Na diet, aiming <3g Na - dietician should be involved
- Reduce EtOH
- Fluid restriction:
- 1.2 - 1.5L/ day, may need to relax the restriction in summer
- determine optimal dry weight
- should weight everyday, if >2kg increase over 2d then see GP/ physician
- can give patient action plan to increase diuretic if there is weight gain
- Psychosocial support, LVEF < 20% predicts major depression
- Sleep apnoea
- adaptive SERVO ventilation is NOT recommended for treatment of central sleep apnoea - N Engl J Med 2015; 373:1095-1105
- Treat obstructive sleep apnoea
- Vaccinate with pneumococcal and yearly influenza vaccines
- Cardiac rehabilitation including multidisciplinary team that involves physiotherapist, occupational therapist, dietician
- Pharmacological measures
- Only proven in the setting of systolic heart failure (decreased ejection fraction)
- Angiotensin-converting enzyme (ACE) inhibitors are recommended for all patients with current or prior symptoms of HF and reduced LVEF, unless contraindicated (Level 1 Recommendation, Level A Evidence)
- Several large trials have proven the benefits of ACEi in the treatment of CCF
- Ang II RB are recommended in patients with current or prior symptoms of HF and reduced LVEF who are ACEI intolerant (Level 1 Recommendation, Level A Evidence)
- Need to up-titrate to dose used in clinical trials
- Candesartan is the only ARB which has clinical trial evidence
- improve morbidity, mortality, increases LVEF and improves remodelling
- No effect of ACE or ARB on diastolic failure, apart from a decease in hospitalisations for heart failure (I-PRESERVE study, used irbesartan)
- Beta - blockers (NYHA II - IV)
- Improve mortality, should not commence in the acute exacerbation phase, usually start prior to discharge
- Carvedilol 6.25mg, 12.5mg, 25mg BD
- Metoprolol CR 23.75mg, 47.5mg, 95mg, 190mg
- Bisoprolol 2.5mg, 5mg, 10mg
- Nebivolol 1.25mg, 5mg, 10mg
- All beta blockers (heart failure beta blockers) have demonstrated a similar risk reduction of 34% in congestive cardiac failure
- COMET study compared regular metoprolol to carvedilol - – mortality benefit for carvedilol – should change to heart failure beta blocker in patients or another beta blocker
- When you start, increment by doubling the dose aiming for target heart failure doses
- eg bisoprolol 10mg, carvedilol 25mg BD
- Aldosterone antagonists (III-IV)
- addition of an aldosterone antagonist is recommended in selected patients with moderately severe to severe symptoms of heart failure and reduced LVEF who can be carefully monitored for preserved renal function and normal potassium concentration
- Spironolactone - has anti-androgen effects
- Eplerenone - selective aldosterone antagonist without anti-androgenic effect, reduces mortality and hospitalisations in the immediate (3 - 14d) post MI period in patients with LV systolic dysfunction and symptoms of HF
- Diuretics
- only for symptomatic improvement
- mortality benefit in the setting of acute pulmonary oedema
- aim for 0.5 - 1kg/day weight loss
- monitor electrolytes
- May have synergistic effect if combining thiazide with frusemide
- Ivabradine
- Blocks the I(f) current - inhibiting the hyper-polarisation activated HCN channel on SA node
- No inotropic effects and no blood pressure lowering effects
- SHIFT study
- Use of ivabridine vs. placebo to improve death/hospitalisation/quality of life
- 18% reduction in primary endpoint of death/heart failure hospitalisation
- Clinical use: patients must be >NYHA II, LVEF < 35%, resting HR > 77, sinus rhythm
- Hydralazine and nitrates
- The combination of hydralazine and nitrates is recommended to improve outcomes for patients self-described as African-Americans, with moderate-severe symptoms on optimal therapy with ACE inhibitors, beta blockers and diuretics (Class I Recommendation and Level B evidence)
- The addition of a combination of hydralazine and a nitrate is reasonable for patients with reduced LVEF who are already taking an ACEI and beta blocker for symptomatic HF and who have persistent symptoms (Class IIa Reccomendation and Level B Evidence)
- A combination of hydralazine and a nitrate might be reasonable in patients with current or prior symptoms of heart failure and reduced LVEF who cannot be given an ACE inhibitor or ARB because of drug intolerance, hypotension or renal insufficiency (Class IIb Recommendation, Level C Evidence)
- Digoxin
- good for symptom control
- Inotropes
- commonly used ones include milrinone and dobutamine - they increase mortality, therefore should only be used as a bridging agent
- levosimenden can also be used, it is a calcium channel sensitiser.
- New agents:
- A new therapeutic class of agents acting on the RAAS and the neutral endopeptidase system has been developed [angiotensin receptor neprilysin inhibitor (ARNI)].
- Valsartan and sacubitril (neprilysin inhibitor, increases naturetic peptides, bradykinin and other peptides --> higher circulation of ANP, BNP --> increase diuresis, natriuresis, myocardial relaxation and anti-remodelling)
- superiority of sacubitril/valsartan over enalapril in the PARADIGM-HF trial
- A new therapeutic class of agents acting on the RAAS and the neutral endopeptidase system has been developed [angiotensin receptor neprilysin inhibitor (ARNI)].
- Devices
- left ventricular assist devices - as a bridge to transplantation
- Biventricular pacing
- Improve quality of life and prognosis
- Patients with LVEF less than or equal to 35%, sinus rhythm and symptomatic (class II >) despite recommended, optimal medical therapy and who have cardiac dysynchrony, which is currently defined as a QRS duration greater than or equal to 0.15 seconds + LBBB morphology should receive cardiac resynchronisation therapy, with or without an ICD, unless contraindicated
- pts with LBBB and QRS > 0.15 benefit the most in trials
- ICD
- A high proportion of deaths among patients with HF, especially those with milder symptoms, occur suddenly and unexpectedly. Many of these are due to electrical disturbances, including ventricular arrhythmias, bradycardia and asystole
- Improve prognosis from sudden cardiac death
- EF < 30-35%
- A cardioverter-defibrillator (ICD) is recommended as secondary prevention to prolong survival in patients with current or prior symptoms of HF and reduced LVEF who have a history of cardiac arrest, ventricular fibrillation or haemodynamically destabilising VT (Level I Recommendation, Class A Evidence)
- ICD therapy is recommended for primary prevention of sudden cardiac death to reduce total mortality in patients with non-ischaemic dilated cardiomyopathy or ischaemic heart disease at least 40 days post myocardial infarction, have an LVEF less than or equal to 35%, with NYHA function class II or III symptoms while receiving chronic optimal medical therapy, and who have reasonable expectation of survival with a good functional status for more than 1 year (Level 1 Recommendation, Class A Evidence)
- A high proportion of deaths among patients with HF, especially those with milder symptoms, occur suddenly and unexpectedly. Many of these are due to electrical disturbances, including ventricular arrhythmias, bradycardia and asystole
Hypertension
Definitions
- Office BP: Average of 2 or more readings on at least 2 or more visits
- Normal BP = systolic <120, diastolic < 80mmHg
- Pre-hypertension = systolic 120-139, diastolic 80-89mmHg
- Hypertension = systolic >140, diastolic >90
- Ambulatory 24hr BP: HTN defined as average ≥ 130/80mmHg. This is the preferred method for Dx
- Age of diagnosis
- Secondary causes
- Complications
- Treatments to date
- Abdominal bruit for RAS
- Fundoscopy for Hypertensive retinopathy
- Endocrine specific examinations
- Primary – combination of age, obesity, FHx, renal function, salt in diet, EtOH, physical inactivity, DM, Chol
- Secondary
- Renal artery stenosis
- Renal artery doppler
- Renal parenchymal disease
- Creatinine level
- Alb/creat ratio
- Hyperaldosteronism (Conn’s syndrome)
- Triad of hypertension/ hypokalaemia/ metabolic alkalosis
- Renin/aldosterone ratio
- Phaeochromocytoma
- Paroxysms of HTN a/w headache/ palps/diaphoresis
- 24hr urinary metanephrines + catecholamines
- Plasma metanephrines
- Cushing’s syndrome
- Cortisol level (late night salivary)
- 24 hr urinary cortisol
- Hyperthyroidism
- Acromegaly
- OSA
- Sleep study if clinical suspicion
- Drug induced hypertension
- NSAIDS
- OCP
- Steroids
- TCA, SSRIs
- Cyclosporin
- Renal artery stenosis
- Ix for secondary causes is only performed in certain patients:
- Young or very old onset of HTN
- Abrupt onset with previously normal BP
- Presentation with stage II HTN
- Clinical suggestion of secondary cause
- Ix for complications
- ECG/ ECHO/ fundoscopy
- Goals according to national heart foundation
- General population ≤140/90
- Diabetics or patients with microalbuminuria ≤130/80
- although this recent study from BMJ - Treatment provided no benefit — and caused harm — in patients with systolic blood pressure <140 mm Hg BMJ 2016 352:i717
- More recently, SPRINT trial suggests that in patients without diabetes:
- "targeting a systolic blood pressure of less than 120 mm Hg, as compared with less than 140 mm Hg, resulted in lower rates of fatal and nonfatal major cardiovascular events and death from any cause, although significantly higher rates of some adverse events were observed in the intensive-treatment group" - N Engl J Med 2015; 373:2103-2116
- Non-pharmacological measures:
- Low salt diet (<2.4g/day). Adopt the DASH diet
- Exercise – 30min mod intensity 4 times per week
- Avoid alcohol
- Stop smoking
- OSA management
- Pharmacological measures
- Primary prevention: assess CVD risk using Framingham risk equation
- High risk – treat
- Moderate risk – consider antihypertensive if fails 3-6months of lifestyle interventions
- Although recent HOPE-3 trial: antihypertensive therapy reduced cardiovascular events in patients with mild hypertension and low overall cardiovascular risk - N Engl J Med 2016; 374:2021-2031
- Low risk – Consider if BP persistently ≥160/100
- Primary prevention: assess CVD risk using Framingham risk equation
- In general population, start drug therapy with any one of the following: See below image BMJ 2016;352:i101
- ACE i
- ARB
- CCB
- Low dose thiazide
- In diabetics or CKD patients, start with an ACEi or ARB
- If monotherapy does not achieve goal, add a second agent from a different class
- If dual therapy does not achieve goal, add a third
- If BP not responding:
- Check for non-adherance
- Undiagnosed secondary causes
- Hypertensive effects of other drugs
- High salt intake
- White coat hypertension
- Resistant HTN
- Defined as HTN that fails to respond to an appropriate 3 drug regimen (including a diuretic)
- Look again for reversible secondary causes
- Add more agents from different classes
- Renal denervation has NOT been established as an effective treatment for resistant HTN (SIMPLICITY-HTN-3)
Secondary prevention in cardiovascular medicine
- Vaccinations
- Meta-analysis of small trials showed 36% reduction in major cardiovascular events, benefiting patients more with recent ACS than stable CAD
- Smoking cessation
- Reduces all cause mortality in CHD pts by 36% in large meta-analysis
- Exercise based cardiac rehabilitation
- Cochrane meta-analysis showing 20% all cause mortality reduction and 26% cardiovascular mortality reduction
- Weight loss
- Patients BMI>25 OR Men waist circ >94cm (Asians 90cm) and >80cm females.
- Epidemiology shows association with cardiovascular mortality as BMI goes up, AND evidence shows that even with normal BMI, all cause mortality goes up with increasing waist circ.
- On multivariable analysis, there was a graded increase in the risk of death from cardiovascular causes and all causes that started among participants in the group that was in the 50th to 74th percentiles of BMI.
- Hazard ratios in the obese group (≥95th percentile for BMI), as compared with the reference group in the 5th to 24th percentiles, were 4.9 (95% confidence interval [CI], 3.9 to 6.1) for death from coronary heart disease, 2.6 (95% CI, 1.7 to 4.1) for death from stroke, 2.1 (95% CI, 1.5 to 2.9) for sudden death, and 3.5 (95% CI, 2.9 to 4.1) for death from total cardiovascular causes, after adjustment for sex, age, birth year, sociodemographic characteristics, and height. DOI: 10.1056/NEJMoa1503840
- Limited evidence for cardiovascular outcomes after weight loss interventions but risk factor improvements have been demonstrated
- Exercise
- 30mins most day of moderate physical activity, if not every day
- Favourable reductions in risk factors and psychosocial wellbeing
- Multiple cohort studies reporting cardiovascular morbidity and mortality reductions
- Fish oil
- Recommendation 1g fish oils daily
- Capsules/ liquid for those with elevated triglycerides
- Systematic review 2012 found no benefit in primary cardiovascular endpoint in study
- JELIS study: primary prevention study had some evidence
- GISSI study: had some evidence for secondary prevention
- Diet
- DASH diet: more fruits and vegetables show reduction in various cardiovascular outcomes in multiple cohort studies.
- Mediterranean diet reduces major vascular events by 30% in large primary prevention trial amongst patients at high risk of ACS
- A high-fat Mediterranean diet doesn't lead to weight gain — rather, it might help with weight loss - PREDIMED study published in the Lancet Diabetes and Endocrinology
- Fibrates
- Major effects of the fibrates are to lower serum triglycerides (by 35 to 50 percent) and raise serum high-density lipoprotein (HDL)
- Fenofibrates can be used with statin, other fibrates not to be used
- Effective in prevention of cardiovascular events without clear mortality reduction. Recommendation based on meta-analysis of secondary prevention trials in patients with established dyslipidaemia (hypertrigs and low HDL-C)
- Additional pronounced microvascular benefits in patients with DM (decrease progression of retinopathy, need for amputations and progression of nephropathy above and beyond baseline lipid values
- Statins
- Strong established benefit for secondary prevention after a vascular event, with high dose favoured to low dose, irrespective of LDL-C
- Heart foundation guidelines like LDL-C <1.8mM
- Mod-high risk patients may benefit from primary prevention: primary prevention trials such as WOSCOPS trial have found substantial reductions in cardiovascular events without increases in non-cardiovascular mortality, but absolute benefit in primary prevention lower than is for secondary prevention
- HOPE-3 trial - intermediate risk population of diverse ethnicity given rosuvastatin 10mg vs placebo. Intervention group showed reduction in cardiovascular events compared to placebo
- Non-statin therapy no evidence in primary prevention, and can increase non-cardiovascular mortality
- IMPROVE-IT: When added to statin therapy (simvastatin 40mg), ezetimibe resulted in incremental lowering of LDL cholesterol levels and improved cardiovascular outcomes. People were eligible for randomisation if LDL (1.3 - 3.2 mM) - N Engl J Med 2015; 372:2387-2397
- Aspirin
- Low dose aspirin has overwhelming evidence for use in secondary prevention of cardiovascular events, no benefit of high dose aspirin
- Should be continued indefinitely
- Extra cranial bleeding risk 169% compared to control
- "Based on evidence from nine large-scale primary prevention trials of men and women without established cardiovascular disease (CVD), aspirin produces a statistically significant and clinically important reduction in the risk of a first myocardial infarction (MI), but not stroke or cardiovascular death " However this is at the expense of an increase in GI and extracranial bleed
- ACE/ ARB
- Use in 0-36hrs is very important, and use over long time has evidence
- Evidence for use in patients with MI both with preserved EF and impaired EF
- No additive benefit of combining ACE/ARB but increased S/E
- GFR usually falls on initiation but it is still Reno-protective and used in patients with CKD
- Beta-blocker
- More evidence for secondary prevention after STEMI compared to N-STEMI
- Systematic review of efficacy in secondary prevention trials found beta-blockers to reduce all-cause mortality
- Effect likely to be over and above heart rate reduction, as ibavradine did not have the same effect
- Controversy remains about optimum duration, with guidelines suggesting re-appraisal after 3 years in patients with preserved systolic function
- PY12 inhibitors
- Any patient with ACS regardless of revascularisation status be treated with DAPT for 12/12
- Ticagrelor/ prasugrel show evidence in comparison to clopidogrel, prasugrel with caution in patients >75 or less 60kg weigh
- Aldosterone antagonists
- Secondary prevention really only for heart failure patients of any aetiology OR MI patients (evidence best in STEMI) with LVEF <40% and on other heart failure drugs
- Endocrine effects better for eplerenone compared to spironolactone
- Caution in renal failure
Dyslipidaemia
Causes
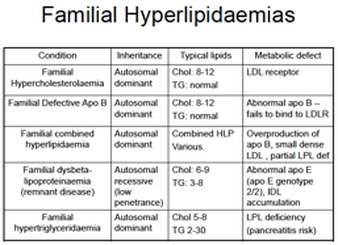
- Primary – familial hyperlipidaemias
- Secondary
- Type 2 DM
- Obesity
- Hypothyroidism
- Nephrotic Syndrome
- ETOH
- Pregnancy
- Corticosteroid excess
- Immunosuppressive agents
- Xanthelasma
- Tendon xanthomas à pathognomonic for FH
- Corneal arcus
- BMI +/- Waist circumference
- Fasting Cholesterol levels including:
- Total cholesterol
- LDL/ HDL cholesterol
- Triglycerides
- TFT
- BSL
- HbA1c
- Goals according to heart foundation
- Total cholesterol <4.0
- LDL cholesterol <2.0 (or <1.8 if very high risk)
- HDL cholesterol >1.0
- Triglycerides <2.0
- Non-pharmacological measures
- Diet
- Reduce saturated and trans fats
- Replace saturated fats with monounsaturated and polyunsaturated fats
- Increase fruit and vegetables and soluble fibre
- Introduce plant sterol-enriched milk, margarine or cheese
- Exercise
- 30min moderate intensity 4 times per week
- 30min moderate intensity 4 times per week
- Smoking cessation
- Diet
- Pharmacological
- All patients should receive secondary prevention with statins
- Consider addition of ezetimibe to statin therapy for added cardiovascular beneifts and reduction in LDL
- Primary prevention
- calculate CVD risk using Framingham risk equation and use lipid lowering Rx if:
- High absolute CVD risk (>15% over 5yrs)
- Familial hypercholesterolaemia
- DM + age >60 or microalbuminuria
- CKD
- BP >180/110
- Chol >7.5
- Intermediate risk (10-15% risk over 5yrs) + family Hx of premature CAD or high risk population (Indigenous/ Islander)
- High absolute CVD risk (>15% over 5yrs)
- PBS allows statin use for any high risk patient or for secondary prevention
- calculate CVD risk using Framingham risk equation and use lipid lowering Rx if:
- Drugs
- Statins - Titrate dose every 4-8 weeks, Increased risk of myositis if also on drugs which inhibit CYP3A4: cyclosporine, azoles antifungals, and certain macrolides
- ezetimibe - as discussed. Second line agent, can be added on to a statin, especially post ACS (IMPROVE-IT)
- nicotinic acid - no convincing evidence, reduces LDL + triglycerides + lipoprotein (a)
- fibrates - second line agents, added to statin therapy or if statin intolerant. Reduces trigs and increases HDL. Sparse evidence
- PCSK6 inhibitors - not on PBS
- OSLER trial N Engl J Med 2015; 372:1500-1509. Reduced the incidence of cardiovascular events for evolocumab
- ODYSSEY LONG TERM - N Engl J Med 2015; 372:1489-1499. Alirocumab reduced LDL when combined to high dose statin in patients at high risk, post hoc analysis showed reduction in cardiovascular events with addition of alirocumab
- OSLER trial N Engl J Med 2015; 372:1500-1509. Reduced the incidence of cardiovascular events for evolocumab
- All patients should receive secondary prevention with statins
Heart Transplantation
Indications
- Refractory heart failure requiring continuous inotropic support
- Cardiogenic shock requiring mechanical assistance with, at worst, reversible end-organ damage
- Congestive heart failure, New York Heart Association (NYHA) Class III or IV symptoms, with objective evidence of impaired functional capacity (peak oxygen consumption <12 mL/kg/min), despite optimal medical therapy
- Refractory angina, despite maximal medical therapy, and not amenable to revascularization
- Refractory life-threatening ventricular arrhythmias, despite maximal antiarrhythmic therapy by all appropriate conventional medical and surgical modalities (multiple firings from an ICD for documented VT and VF)
- Congenital heart disease with progressive ventricular failure that is not amenable to conventional surgical repair
- Severe hypertrophic or restrictive cardiomyopathy, with NYHA Class IV symptoms
- Fixed pulmonary HTN (trans-pulmonary gradient >15mmHg)
- Active or recent malignancy within 5 years
- Age >65
- BMI>35
- Active systemic infection/inflammation
- HIV/ HBV and HCV are relative CI
- Diabetes with end organ damage
- Irreversible renal or hepatic failure (eGFR <40ml/Min)
- Psychosocial instability, substance abuse
- Inability to comply with follow up medical care
- Recent PE (<6weeks)
- prior to Transplant - 40% of patients will have a LVAD as a bridge to Transplant
- Indicated if repeated admissions to hospital for decompensated HF
- Main SE = thrombosis, infection
- Need Warfarin + at least one antiplatelet
- General – Height, Weight, BMI
- Side effects of immunosuppression:
- Cushingoid due to steroids
- Cyclosporine - Gum hypertrophy and hair
- Tacro – DM
- Skin cancers
- Neck – Small scars in neck (endomyocardial biopsy scar)
- Chest
- Median sternotomy scar
- Signs of HF and Pericarditis
- Pre-transplant
- ECG, TTE (PulmHTN?), Gated Heart Pool Scan, 24hr Holter
- Coronary Angiography
- Carotid duplex
- Right heart cath to determine TransPulmonary Gradient - Cannot transplant if PHTN; Transplanting new heart into a high pressure system --> RV failure
- TPG = PAP – mean PCWP
- Normal TPG < 12
- TPG > 15 : Not for transplant
- If TPG 12-15, commence CCB and repeat angio --> if <12 then TXP
- TPG = PAP – mean PCWP
- Consider endomyocardial biopsy
- Viral serology
- EBV/ CMV/ HIV/ HBV/ HCV
- Toxoplasmosis serology
- CXR, ABGs, spirometry, Lung Funciton (DLCO)
- Sleep Study if OSA suspected
- Age appropriate malignancy screen
- ABO
- Donor cross match
- HLA tissue typing
- Transplant CNC coordinator
- OPG & Dental consults as required
- Psychiatric and SW as required
- Dietician
- Peri-transplant care
- endomyocardial biopsy looking for signs of acute cellular/ vascular rejection
- q 1 week for 1m
- q 2 weeks for 2m
- q 1 month for 6m
- Then at 8m and 12m
- Surveil for symptoms of rejection - noting that most rejection episodes occur early - almost 50% of the rejection episodes occur in the first 2 to 3 months
- Hypotension SOB, Arrhythmias (AF/Flutter)
- Oedema
- Unexplained fever/flu like illness, pleuritic CP
- Reduced LVEF (TTE/GHPS)
- ECG abnormalities: decr ECG voltge (myocardial oedema)
- endomyocardial biopsy looking for signs of acute cellular/ vascular rejection
- Mx of acute rejection
- Cardiac biopsy - histological grade 2 - 3 require treatment, based on lymphocytic infiltrate
- Pulsed IV Methylpred for 3 days then wean of increased pred dose (60mg)
- Anti-thymocyte globulin (ATG) may be needed in severe cases
- Mx of chronic rejection
- Coronary artery vasculopathy represents a chronic rejection phenomenon (5 year incidence 30%, 10 year incidence 50%)
- Diffuse progressive concentric intimal hyperplasia
- Coronary artery intimal hyperplasia
- Usually asymptomatic as the Tx heart has been denervated
- Patients require routine coronary angiograms on a biannual basis to look for CAD
- Rx: consider changing from CnI to mTOR, use pravastatin, normally started immediately - not metabolised via CYP therefore less interactions
- Coronary artery vasculopathy represents a chronic rejection phenomenon (5 year incidence 30%, 10 year incidence 50%)
- Mx of increased risk of malignancy
- Skin most common (BCC and SCC)
- Sun protection, derm review
- Consider change to mTOR inhibitor which has lower rates of cutaneous malignancy
- PTLD - Mx by decreasing immunosupression, some will need rituximab or high intensity chemotherapy regimes
- Skin most common (BCC and SCC)
- Mx of increased risk of infection secondary to baseline immunosupression
- Vaccination up to date prior to transplant
- No live vaccines
- Prompt investigation and treatment
- Prophylaxis
- PCP (Bactrim DS, Mon/Wed/Fri)
- Aspergillus (Itraconazole 3m post transplant)
- CMV (if mismatch, valganciclovir for 3/12)
- Other issues include NODAT (new onset diabetes after Transplant), osteoporosis, renal dysfunction
- Median survival 10 years (international), 14 years (AUS)
- Causes of death post transplant:
- Infection most common in first yr
- Cardiac allograft vasculopathy is common at 3-5yrs
- Malignancy becomes the most common cause from 3-10yrs
- Survival
- 1 year – 90%
- 5 year – 75%
- 10 year – 60%