Chronic Liver Disease
Presentation
- Ask when pt was diagnosed
- Symptoms at diagnosis - lethargy, fatigue, abdominal distension, hypervolemia, pruritis, haemetemesis, malena, confusion, jaundice, movement disorder, psychosis, blistering skin reaction of porphyria cuteanea tarda, joint pains, diabetes, bronzing pigmentation, slate-green pigmentation of PBC, other auto-immune problems, sjogren's syndrome, SBP, infection, loss of libido, abdominal pain and fever in acute hepatitis, Hx of ulcerative colitis (PSC)
- May have been diagnosed after presenting with a complication of decompensation - ascites, SBP, encephalopathy, variceal bleeding
- For aetiology
- autoimmune profile, immunoglobulins, genetic tests, Cu/ ceruloplasmin studies, viral serology, metabolics
- Liver biopsy
- For complications
- Diagnostic paracentecis - SAAG >11 for portal hypertension related ascites
- Upper endoscopy for varices
- US +/- triple or quad phase CT scan for hepatoma
- Renal biopsy if membranoproliferative GN suspected
- ECHO shunt studies, right heart catheters for hepatopulmonary syndrome or porto-pulmonary hypertension
- For prognistication
- MELD score
- Childs Pugh
- Maddry's score for acute alcoholic hepatitis
- Depends on aetiology
- Viral hepatitis: vertical transmission, tattoos, parenteral, faecal-oral
- Drugs: MTX, amiodarone, isoniazid, PTU, flucloxacillin, halothane, paracetamol, EtOH [significant intake required for males, less for females]
- Metabolic risk factors: female, dyslipidaemia esp triglycerides, obesity, waist circumference, diabetes
- Autoimmune risk profile
- Family history of wilson's disease, haemochromatosis
- Ulcerative colitis
- All pts should have hep A and hep B vaccines
- Aetiology specific Rx:
- NASH: weight loss targeted to 0.5-1kg/week, vitamin E 400 - 800IU if not diabetic and evidence of fibrosis, statins safe to use, modify risk factors
- Alcohol - Rx dependence, abstinence
- HCV - new PBS listings for direct acting antiviral agents, high chance of recurrence post transplant, minimise with steroid free regime. Rx for 12 weeks, if cirrhotic 24 weeks and if had prior Rx 24 weeks.
- HBV - Rx in immune escape or immune clearance phase to target viral replication and avoid necro-inflammatory pathology. This is evidenced by high DNA levels, Hep E Ag + and rising ALT/ AST - Rx include peg IFN vs entacavir/ tenofovir. Pre-treat prior to transplantation then give Hep B Ig to recipient
- PBC - UCDA for all pts
- PSC - UCDA for symptoms of pruritis, surgical stenting and biopsy looking for cholangiocarcinoma, prophylactic Abx if recurrent cholangitis
- Haemochromatosis - asymptomatic and ferritin <500 --> surveillance program with yearly specialist visits, if symptomatic with end organ manifestations, require weekly phlebotomy, targeting ferritin 50 - 100, then maintenance phlebotomy regime. Fe chelation Rx only if pt cannot tolerate phlebotomy
- Wilsons - all pts need Cu chelation therapy with D-penicillamine or trientine, asymptomatic pts may use Zn if do not want Rx.
- Autoimmune: prednisolone +/- azathioprine - with treatment, the 10-year survival rate is approximately 90 percent. Rx indication controversial, but generally recommended if ALT > 10x normal, Igs > 2x normal, or histological features of advanced fibrosis seen
- Of complications:
- Ascites:
- Goal: 0.3 - 0.5kg loss/day
- Non-pharmacological: salt restriction (no added salt or salt restricted diet based upon dietician consultation +/- fluid restriction (start 1.2L then titrate) and nutrition (high protein, will need supplements, in patients may need NG feeding)
- Pharmacological: Start spironolactone and frusemide (50mg : 20mg ratio) and uptitrate. Monitor electrolytes and renal function. Frusemide especially good if pt has oedema. Titration every few days
- Invasive
- Paracentesis can be intermittent for comfort - need albumin cover of conc 20% 100ml per 2L drain, max 10L drain/ day or can be regular program. Make sure not overtly coagulopathic (INR <2.5, plt > 50)
- TIPPS: only if synthetic function ok, not coagulopathic, cardiac function ok (increased venous return can overload frank-starling coupling) and if no PV thrombus
- Encephalopathy
- Goal: prevent deterioration, prevent recurrence
- Non-pharmacological: nutrition and supplementation with branched chain amino acids (hepatamine)
- Pharmacological: Lactulose (BD dosing, titrate to achiwvw 2-3 bowel motions/d), add rifaxamin (must be used in combination). Infection is most common cause, but others include electrolyte dyscrasias esp hypokalaemia, large protein meal and constipation.
- Other considerations: covert encephalopathy - first presents with inversion of sleep: wake cycles, driving considerations, make sure Zn replete (Zn theoretically improves ureagenesis)
- Varices:
- Surveillance - at time of diagnosis of cirrhosis. If small varices can repeat scope in 2 years time
- Primary prophylaxis: Either beta blockade (low dose propanalol, 10mg BD, titrate to aim reduction of 25% resting HR) OR banding program (equivalent) - repeat procedures 6 - 8 weekly until eradicated then repeat scope in 12 months. Give patients BD PPI for 3/52 as converts
- Secondary prophylaxis: beta blockade and banding program. Make sure empirical antibiotics are given
- Intervention: TIPPS - evidence for early on, but remember contraindications (1) encephalopathy and/ or synthetic impairment (bili <50) (2) cardiomyopathy (3) PV thrombus.
- Other considerations: no prophylaxis to be given for gastric varices - Rx with glue
- SBP
- Primary Prophylaxis: if ascitic protein < 15g/L --> quinolones help to increase time to occurence but no clear survival benefit
- Rx: ceftriaxone or tazocin, IV albumin to reduce risk of HRS
- Secondary prophylaxis: Prophylactic treatment following episode reduces recurrence (untreated ~70% at 1 year) and improves survival
- HCC surveillance program
- 6 monthly US +/- AFP once cirrhotic
- HBV pts also qualify (Asian, african americans)
- Surgical: Curative if 3 x <3cm, 1 x <5cm --> transplantation and if not a candidate, then radiofrequency ablation. If i nodule <2cm then can have hepatic resection
- Nutriton
- Frequent meals 4 - 7/d
- low Na (<2g)
- Ascites:
Inflammatory Bowel Disease
Clinicopathologic differences:
- Ulcerative colitis: Inflammation up to submucosa, starts at the rectum, extends proximally, no skip lesions: histologically characterized by goblet cell depletion, crypt distortion, cryptitis, crypt abscess. Note acute inflammation see neutrophils, chronic = lymphoplasmacytic infiltrate in colon.
- Rectosigmoid > left sided > pancolitis
- Crohn’s disease: segmental, transmural inflammation with different phenotypes: inflammatory, structuring, penetrating, granulomas are pathognomonic.
- Terminal ileum only 49%, colon only 20%, upper GIT involvement =4%
- Smoking makes Chron’s disease worse [quit and reduce relapse rates by 65%] but protective for UC
- Genes: NOD2/CARD15 causes abnormality in sensing luminal bacteria [defect making more bacteria getting through initial defence], leading to inappropriate activation of immune response to bacteria in genetically susceptible host
- Appendicectomy protective [esp against UC]
- Poor prognosis CD [<40, perianal disease, stricturing phenotype, fistulising disease, weight loss, steroids for first flare]
- Extraintestinal manifestations independent of GI activity [uveitis + pyoderma gangrenosum + ankylosing spondylitis + PSC + kidney stones], paralleling GI activity [episcleritis, large joint arthritis, erythema nodosum, oral ulcers]
- Dx [accurate Dx is important b/c Rx differ and surgical approaches may be different]
- Aids to diagnosis: fecal calprotectin [remission calprotectin helps predict when relapses occur, also tells us if there is inflammation], inflammatory markers, ASCA [CD], anti-OmpC [CD], p-ANCA [UC]
- Chron’s macroscopy: cobblestoning [oedema around ulcers], deep fissures, longitudinal ulcers
- Ulcerative macroscopy: spontaneous bleeding, shallow erosions and ulcers, pseudopolyps
- Imaging: Use Small bowel MRI [contrast concerns in the young] esp if considering small bowel chron’s, CT abdomen [bowel wall thickening, fistulas, abscess, Image SIJs [Sero-negative arthritis]
- Disease activity [CDAI for chron’s, Montreal classification for UC]
- Phenotype for chron’s disease: Age, Location [ileal, ileocolonic, colonic, upper], Behaviour [non-penetrating + non-stricturing vs structuring vs penetrating]
- Phenotype for Ulcerative colitis: Extent [proctitis, left-sided up to splenic flexure and pancolitis], Severity [# of stools, blood, Hb, ESR, temperature, PR]
- 5-ASA backbone of therapy
- Overwhelming endpoint --> obtain endoscopic remission and mucosal healing [should be the goal of Rx]
- 5-ASAs: Sulfasalazine, mesalazine, olsalazine
- PO and oral prep, SE = male oligospermia, hypersensitivity, anemia, folate deficiency, diarrhoea, headache, rash, agranulocytosis, hepatitis, pancreatitis.
- Sulfasalazine before mesalazine [PBS], although sulfasalazine associated with greater side effects
- For Induction AND maintenance Ulcerative Colitis, no role maintenance Chron’s disease
- If proctitis and L sided disease [Topical ASA > ASA but Topical + oral ASA > topical ASA, can also have topical steroids + topical ASA], If pancolitis --> topical [enema] + oral. Enemas get to splenic flexure, foams get to 25cm and suppositories get to 7cm.
- Once daily regime as effective therefore do this!
- Rectal ASA > rectal steroids for left sided disease.
- Corticosteroids --> only for disease flares in mode/ severe disease
- Thiopurines (azathioprine and 6-MP). Here only used in maintenance of remission as onset of action takes too long.
- First do TPMT levels: (1) mutant/ mutant [level < 5] = avoid drug OR very low dose because high levels of 6-TG as not metabolised (2) mutant/ wt [level 5 - 8] = give 1/3 dose (3) wt/ wt [level > 8] = give full dose drug
- SE = nausea, neutropenia, hepatitis, fever, rash, arthritis, hepatitis [6-MMP metabolite]. Rare S/E = hepatosplenic T Cell Lymphoma, esp if with anti-TNF alpha agents
- Thioguanine metabolite levels help with titration based on metabolism
- 6-TG [active metabolite], 6-MMP [inactive hepatotoxin]
- If low 6-TG, low 6-MMP = non-adhearance, if low 6-TG, high 6-MMP = predominant TPMP metabolism, can give allopurinol + 1/3 thiopurine dose to increase shunting to 6-TG
- Evolving evidence for use of methotrexate in IBD, especially from meteor trial, but results controversial and not widely used
- Anti TNF-alpha Rx --> evidence for use if steroid refractory and have tried other non-biological DMARD
- Vaccinate prior, and have live vaccines done 3 weeks prior to initiation. Cannot have live vaccines until 3 months of completing treatment
- S/E --> re-activation of latent TB. If LTBI found [IGRA, mantoux test], treat with 9/12 Isoniazid Rx. Demyelination syndromes can also occur
- Must combine with MTX or azathioprine, prevents anti drug antibodies and achieves synergy
- Vedolizumab [a4b7 integrin] --> UC in induction and maintenance of remission
- Acute severe colitis [based on trulove and witt's criterion]
- Admit, hydrocort 100mg qid, surgical consult, assess day 3 --> if markers of severity persist [number of bowel motions, CRP], start cyclosporin infusion [or infliximab] for 7 - 10d. If failing, or complicated by toxic megacolon, patient requires subtotal colectomy. Exclude other causes such as C. diff, CMV colitis
- Exclusive enteral nutrition --> mainly for children but has limited evidence for adults (liquid feed) - 6 to 8 weeks, especially if there is a contraindication to corticosteroids.
- Corticosteroids
- prednis(ol)one 40 to 60 mg (child: 1 to 2 mg/kg up to 40 to 60 mg) orally, daily until clinical response, then gradually reduce over 8 to 12 weeks to cease
- budesonide 9mg orally for ileocaecal disease
- hydrocortisone 100mg qid if severe disease
- For induction if steroid refractory can use anti-TNF alpha agents
- TNF-alpha agents have evidence in peri-anal, fistulising, post-op prevention
- If steroid dependent, can trial: azathioprine, mercaptopurine or methotrexate + folic acid
- Surgery
- Fibrotic stricture, fistulae [medical and surgical], abscess, perforation are indications, 60% CD need Sx within 10y, infliximab highly effective at preventing post-op recurrence
- Cancer screening guidelines [note NEJM2015]
- Depends on PSC [if present at time of Dx and then annually thereafter], duration of colitis modified by extent of colitis [at 8y from Dx if >1/3 colon, 12y if <1/3], and how often determined based on disease activity [active = yrly, inactive 3yrly, last 2 colonoscopies normal = 5yrly], other risk factors [PSC = yrly, FHx <50 first deg, stricture, pseudopolyps, past dysplasia = yrly, otherwise 3yrly]
Liver Transplantation
History
- Reason for transplantation (aetiology of liver disease, presence of decompensation, complications, MELD score, presence of HCC)
- If in pre-transplantation phase, determine work-up. This includes the following
- MELD score >10, or Na-MELD score. Presence of HCC and Milan's criterion for OTLx
- single tumor up to 5 cm or up to three tumors with less than 3 cm and no major vascular invasion such as portal and hepatic vein, as determined by imaging studies
- Cardiopulmonary fitness for surgery: This is an extensive surgery therefore a patient must be suitable enough to tolerate the insult - anticipating blood loss, haemodynamic insults etc
- Peri-operative nutrition
- Cardiac: ECG, Echo ± dobutamine stress echo
- Pulmonary: ABG, formal lung function, contrast echo (bubble / shunt study ?HPS)
- Triple phase CT: Vascular anatomy ± HCC
- Ascertain suitability for post-transplantation care
- Tolerability of ongoing immunosupression: Prior malignancy >5y, Viral serology (HBV / HCV / HIV / CMV)
- Psychosocial fitness
- MELD score >10, or Na-MELD score. Presence of HCC and Milan's criterion for OTLx
- Determine surgical details
- recipient operation consists of total hepatectomy of the native liver followed by implantation of the donor liver
- Orthotopic versus split liver transplant (transplanting one donor liver into two recipients, can be split in two different ways - one where there is a adult and paediatric and the other way in which there is two adult)
- Livers are ABO matched but not HLA matched
- Duct to duct versus Roux-en-Y
- Surgical recovery, days in ICU
- Immunosuppression
- Steroids: ?pulse, ?dose history
- CNI: cyclosporine or tacro
- Anti proliferative: MMF or AZA
- mTOR: Sirolimus or everolimus
- Infection prophylaxis
- Bactrim for 12 months
- CMV: recipient + 3 months; discordant 6 months - use valganciclovir
- Treatment of metabolic complications
- Progress
- Complications
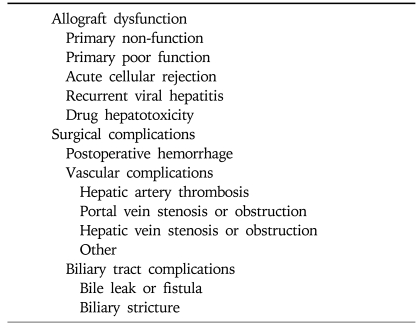
- Immediate post-operative complications include the following (see table below)
- daily routine Doppler ultrasound exam should be performed to exclude vascular complications such as hepatic artery thrombosis, portal and hepatic vein stenosis or obstruction
- Medium term complications include biliary stricture, acute rejection, infection, disease recurrence
- Long term complications include: metabolic risk factors, cancer, bone health, infections such as CMV, pneumocystis, disease recurrence
- Side-effects of immunosuppressant drugs
Post transplant infection/ prophylaxis
1. Immunosuppression
Follow up post Transplant
- PCP prophylaxis
- Bactrim Double strength ½ tablet three times weekly for 12 months
- If intolerant of Bactrim then can use nebulised pentamidine given once monthly
- CMV Disease/ prophylaxis
- Recipient positive then 3/12 oral valganciclovir
- Sero-discordant (recipient negative, donor positive) then oral valganciclovir 6/12
- both sero-negative: monitor only
- Clinical features of CMV disease include, Febrile flu like illness, Leukopenia + Atypical lymphocytes, Diarrhoea, Respiratory symptoms, Hepatitis
- CMV treatment (1) Ganciclovir IV for 1-2/52 and then (2) Followed by Valganciclovir for 3/12
- Fungal infections
- Most common is candida
- Fungal prophylaxis with fluconazole is used only in certain patients
- Complicated Tx
- Acute hepatic failure
- Patients with long term Abx use prior to Tx
1. Immunosuppression
- Maintain graft function, prevent rejection and balance risk of infection
- Management:
- Monitor LFTs, EUC and CNI drug levels
- Monitor for complications of immunosuppression:
- Diabetes - HbA1C --> tac increases DM > cyclosporin
- HTN - Screen for and Rx HTN (CNIs are a/w HTN)
- Malignancies
- Osteoporosis
- Skin checks
- Aim: Aggressive control of vascular RFs
- Management:
- Check:
- Fasting bsl and HbA1C
- Lipids
- BP
- Renal function
- Management:
- Non-pharm = Diet and exercise
- Diabetic control
- Statins
- Obesity management
- HTN management
- Check:
- Caused by CLD and long term prednisone
- Aim: Identify and manage OP
- Management:
- Check:
- 25(OH)D level, aim >75
- BMD measured every 1-2 years
- If T score < -1.5 Rx with bisphosphonate
- Check:
- Screen for and manage malignancies
- Skin checks at dermatologist
- Low index of suspicion for solid tumour
- Post transplant lymphoproliferative disease (PTLD)
- serious and potentially fatal complications of chronic immunosuppression in solid organ and hematopoietic cell (HCT) transplant recipients
- approximately 1 percent in the transplant population, highest for heart and lung transplant patients
- Mostly related to proliferation of EBV-positive B cells in the setting of chronic T cell immunosuppression but EBV negative B cells and T cell lymphomas can also occur
- prevention of PTLD largely relies upon limiting patient exposure to aggressive immunosuppressive regimens, aggressive withdrawal and tapering of agents required for graft acceptance, and anti-viral prophylaxis
- Can monitor EBV titres, and if rising, can decrease immunosupression and/ or Rx with rituximab
- serious and potentially fatal complications of chronic immunosuppression in solid organ and hematopoietic cell (HCT) transplant recipients
- Monitor tacrolimus and cyclosporine levels
- Biopsy if evidence of graft dysfunction
- Treat rejection with pulse of methylpred +/- increase background immunosuppression
- Investigate cholestatic LFTs with:
- USS/ CT/ MRCP
- ERCP +/- stenting
- Management:
- ERCP + stent
- PTC
- Re-fashion anastomosis
- Prophylactic antibiotics
- Re-transplant
- Almost all diseases recur with the exception of metabolic diseases
- HCV recurrence is universal with mean time to recurrent cirrhosis of 7yrs.
- Patients Rx for acute cellular rejection and those with older donor livers have earlier recurrence.
- HBV is treated with lifelong antivirals (Entecavir) which prevents disease recurrence very effectively
- PSC --> 20% develop recurrence
- PBC --> slowly progressive graft disease so mortality is rare
Follow up post Transplant
- Patients are reviewed very frequently:
- Twice Weekly for 1 month
- Weekly from 1-2 months
- Second weekly from 2-3 months
- Monthly from 3-12 months
- Three monthly thereafter