Adherence and Compliance
N Engl J Med 2005; 353:487-497
Assess level of adherence
Assess level of adherence
- Adherence is better terminology than compliance, as the latter assumes the patient is subservient to the doctor, and the former implies a therapeutic alliance
- Ask permissive questions
- “You are on lots of medications, how do you manage to take them everyday”?
- How many days in a week would you miss your medications - why
- Do they use a Webster pack or Dosette box
- What do you do when you forget a tablet? Double dosing?
- Which medications do you not want to take?
- Other non-adherence behaviours
- INR checks
- Missing appointments
- BSL checks
- Directly observed therapy
- Measurement of concentrations of a drug or its metabolite in blood or urine, and detection or measurement in blood of a biologic marker added to the drug formulation
- Indirect methods of measurement of adherence include asking the patient about how easy it is for him or her to take prescribed medication, assessing clinical response, performing pill counts, ascertaining rates of refilling prescriptions, collecting patient questionnaires, using electronic medication monitors, measuring physiologic markers, asking the patient to keep a medication diary
- Patient factors
- Presence of psychological problems, especially depression
- presence of cognitive impairment
- Patients lack of belief in treatment benefits
- Level of education
- Lack of insight into illness
- knowledge of disease process
- missed appointments
- Disease factors
- treatment of asymptomatic disease
- Doctor factors
- inadequate follow-up or discharge planning
- Poor doctor-patient relationship
- Medication factors
- side effects of medications
- cost of medication, co-payment or both
- complexity of treatment
- pill burden
- dosing regime
- presence of barriers to obtaining medications
Improving Adherence
- Open-non judgemental approach
- Addressing multifactorial, multi-dimensional barriers in a co-ordinated multi-disciplinary manner
- Patient education
- Involving patients
- their family members
- engage other practitioners - eg GP and pharmacist
- Simple language
- patient fact sheets
- Engage in patient support groups
- Improve dosing schedules
- use of pillboxes to organize daily doses
- simplifying the regimen to daily dosing
- cues to remind patients to take medications - eg apps, enlisting family members, community nursing
- slow release formulations, transdermal patches, combi-pills
- manage drug side effects
- Access to medications
- Some pharmacies home deliver
- Medication safety net and substituting generic medications
- Compassionate access
- Follow-up
- more regular follow-up appointments
- addressing barriers to follow-up appointment
Fitness for Surgery
"I am concerned about the risks that this major surgery poses for this patients short term peri-operative health". In an attempt to improve his peri-operative outcome, I would like to focus on the following key components..."
Aust Prescr 2014;37:188-91
Cardiac risk
Aust Prescr 2014;37:188-91
Cardiac risk
- Assess functional capacity. If they can climb >1 flight of stairs then they can perform >4 METS
- < 4 METS indicates high risk
- Different types of surgery carry different cardiac risks
- Use tools such as the revised Goldman cardiac risk index
- High risk type of surgery (vascular/ aortic intervention)
- History of ischaemic heart disease (either presence of q waves on ECG, presence of angina, active use of nitrates, Hx of AMI, + exercise stress test)
- note that Hx of coronary vascularisation does not count as a risk factor unless one of the above criterion is satisfied
- Heart failure Hx
- Hx of cerebrovascular disease
- Hx of DM requiring insulin
- Serum Cr > 177
- Each of the above risk factors add to periop cardiac mortality and morbidity, with > 2 goldman risk factors signifying intermediate risk
- If intermediate risk offer non-invasive testing
- Myocardial perfusion imaging
- Fixed defect CER 37%
- Reversible defect ER 24%
- Normal MIBI cardiac event rate (CER): 4%
- Multiple involved segments further increase risk
- + stress test would prompt a strong consideration for PCI
- A recent population-based retrospective cohort study of 264 823 patients showed no benefit in survival or hospital length of stay from rest echocardiography performed within the 6 months before surgery BMJ 2011
- Myocardial perfusion imaging
- For very high risk conditions, the need for emergency surgery often trumps the high perioperative risk in terms of clinical equipoise
- Elective surgery should be differed as below in order to stabilise the patient
- Unstable coronary syndrome - Recent MI or unstable angina within last 6 weeks (optimal > 3 months)
- Recent PCI within 6 weeks (optimal > 3 mnth)
- Decompensated heart failure or significant valvular disease
- Significant arrhythmias
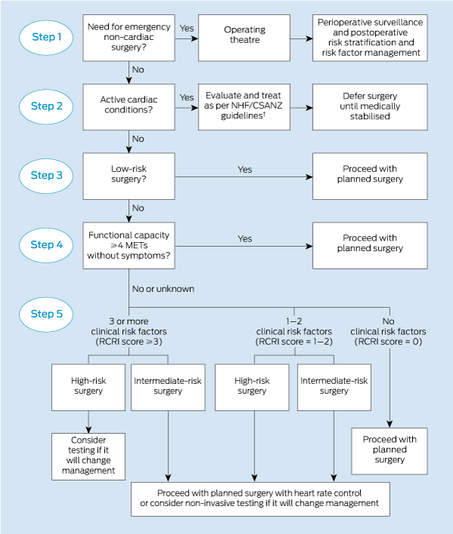
- An effective algorithm (MJA 2013) is shown below
- Risk mitigation in high risk patients proceeding to surgery
- Mixed guidelines. A large meta-analysis that included the POISE trial suggested that beta-blockers increased all cause mortality but the meta-analysis included a lot of low risk patients. Two large retrospective observational studies using propensity-based risk adjustment suggest that β-blockers reduce all-cause inhospital deaths proportionally to increasing cardiac risk
- It is reasonable to start a beta-blocker in high risk patients one month prior to surgery
- Consider coronary revascularisation for patients with proven IHD undergoing high risk procedures (vascular surgery)
- Thoracic and upper abdominal surgery causes impaired pulmonary physiology, with reduction in VC (50 - 60%), reducing FRC by 30%. Risk of pulmonary complications increased by underlying COPD/ asthma
- Smoking increases post-op pulmonary complications (RR 1.7), but need to stop smoking 8 weeks pre-op to reduce risk
- Pulmonary hypertension (mortality OR 3.7-4.5)
- Pre-operative Ix: spirometry has no evidence it helps but it may be useful for the anaesthetist, post-op care and is useful to triage suitability for use of beta-blockers
- Preoperative deep breathing and education reduces post-op pulmonary complications
- Pre-operative interventions: COAD
- Treat pre-operative exacerbations aggressively
- Corticosteroid use does not increase post-op wound infections
- Pre-operative intervention: stop smoking
- Physiological effects seen if stop 48 hours prior to surgery
- Risk of post-op pulmonary complications decreases only after 8 weeks cessation
- Major risk factors for post-operative pneumonia
- Type of surgery: AAA repair (OR 4.29); thoracic surgery (OR 3.92); upper abdominal surgery (OR 2.68); neck surgery (OR 2.30); Neurosurgery (OR 2.14)
- Age: >= 80 (OR 5.63); 70-79 (OR 3.58); 60-69 (OR 2.38)
- Functional status: totally dependent (OR 2.83); partially dependent (OR 1.83)
- Weight loss > 10kg in past 6 months (OR 1.92)
- History of COPD (OR 1.72)
Balancing the risk of immunosupression and infection
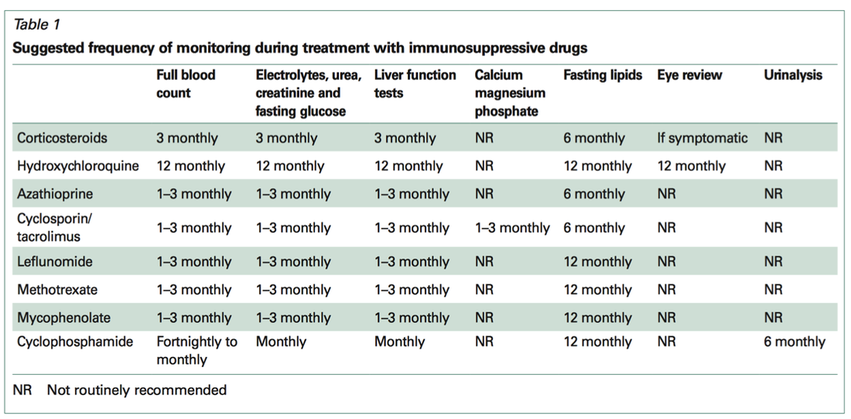
Aust Prescr 2009;32:68-71
General approach
General approach
- Establish that it is a complex management issue, because at one side you have the risks of significant end organ damage posed by a serious condition (or threaten an allograft) but on the other side there is a significant increased risk of mortality secondary to unremitting infection
- The most important thing is to initially establish the risks associated with each variable of the equation
- Always discuss with the patient the risks and benefits
- Risks posed by acute infection
- how acute is the problem?
- note that chronic deep seated infections such as osteomyelitis may be unable to be controlled without lessening immunosuppression
- how severe is the problem? - are there markers of end organ dysfunction?
- can we treat the infection without decreasing the immunosuppression
- some infections are exquisitely immunosensitive, such as PML, BK virus
- how acute is the problem?
- Risks posed by decreasing immunosupression
- how active is the condition - is there an active need for immunosupression
- what is the severity of the condition?
- has it been severe in the past - ie predicting a severe phenotype
- are there other alternatives?
- What are the modifiable risk factors?
- prophylactic antibiotics/ antivirals
- vaccinations?
- avoiding high risk exposure?
- nutrition
- smoking cessation
- look into other reasons for impaired immunity such as autoimmune leukopenia, secondary hypogammaglobulinaemia, HIV
- appropriate level of immunosupression
- therapeutic drug monitoring
- azathioprine and TPMT levels, guanine metabolites
- Drug interactions
- CnIs and CYP inhibitors - eg azoles, statins, diltiazem
- azathioprine and allopurinol
- Methotrexate and bactrim/ trimethoprim
- Glucocorticoids: viruses (esp herpes); fungal; bacterial, usually dose dependent increase in risk
- In C. difficle, corticosteroid use is associated with increased mortality Ther Adv Chronic Dis. 2013 Jul; 4(4): 167–185.
- Rituximab: PML, activation of latent HBV, CMV
- CnI: bacterial; viral esp CMV; fungal
- MMF: Viral infections
- Azathioprine: bacterial infections (esp in setting of leukopaenia); viral infections esp HSV
- TNF inhibitors: reactivation of Hep B; VZV; TB; ? non-TB mycobacteria; fungal infections
Management of Pain
History
- Quantify baseline pain (x/10)
- Quantify exercise tolerance
- Ask about impact on sleep and occupation
- Red Flags - point tenderness, night pain, weight loss, fevers, high CRP, sensory change, bladder/ bowel function
- Effect of chronic pain on function
- Chronic diffuse non-inflammatory soft tissue pain with little diurnal variation
- Diffuse tenderness. No specific examination findings
- Associated symptoms: fatigue, impaired concentration, sleep dysfunction, depression, irritable bowel and irritable bladder
- Management: reassurance, regular aerobic exercise, sleep hygiene, support group
- Pharmacological
- Amitriptyline 10 -> 50mg nocte
- Pregabalin 25mg nocte -> 150mg BD (not PBS listed for this)
- Duloxetine 30mg -> 60mg daily (not PBS listed for this)
- Avoid opioid analgesia
- Multimodal/ multidisciplinary team approach
- Realistic patient expectations, we will not cure but improve function and tolerance
- Utilisation of the WHO Pain pharmacological treatment ladder
- RICE: rest, ice, compression, elevation
- Heat packs, physiotherapy such as hydrotherapy, graded exercise therapy so as to not overdo it
- TENS (Transcutaneous Electrical Nerve Stimulation)
- Disrupts nociception
- Reduces amount of pharmacological Rx required
- Cochrane database 2015 meta-analysis: some mild evidence for use in acute pain vs placebo
- Splints/ orthotics/ braces for immobilisation
- Massage
- Cognitive behavioural therapy
- Important to get rid of idea of “cure” via surgical intervention
- Catastrophising: e.g think they will end up wheelchair bound so there’s not point
- Start with dose and add breakthrough component
- breakthrough calculated as one twelfth to one-sixth of the total daily dose fractionated
- Paracetamol +/- codeine (mild pain)
- Panadol – paracetamol 500mg
- Panadol osteo – long acting form of paracetamol, 665mg taken as ii TDS
- Panadeine – paracetamol 500mg + codeine 8mg
- Panadeine extra – paracetamol 500mg + codeine 15mg
- Panadeine forte – paracetamol 500mg + codeine 30mg
- NSAID – use PRN if possible and give PPI if expect regular use to prevent gastric ulcer. Can try topical
- Non-selective COX inhibitor have lowest CV risk
- Naproxen
- COX-2 inhibitors have lower GI risk
- Celecoxib (Celebrex)
- Meloxicam
- Avoid if “Triple whammy”: ACEI, diuretic
- can use with low dose aspirin, just ensure separation with time
- Non-selective COX inhibitor have lowest CV risk
- Joint injections
- Corticosteroids
- Give symptomatic benefit for 2-3 months
- Corticosteroids
- Tramadol
- Weak opiate receptor agonist + serotonergic and noradrenergic actions
- Start 50mg tds
- Beware of serotonin syndrome if on TCA
- Tapentadol (Palexia SR)
- Centrally acting analgesic with dual mechanism of action (mu receptor agonist 18x weaker than morphine and noradrenaline re-uptake)
- Indications: moderate to severe chronic pain
- Initial dose 50mg BD, maximum dose 250mg BD
- Extensively metabolised (cytochrome P450) --> Inactive metabolites
- Better GI tolerability than oxycodone
- Contraindicated with MAOI
- Potential for serotonin syndrome with TCA, SSRIs, SNRIs, but less so than tramadol
- Abuse and dependency issues exist
- Targin (Oxycodone with Naloxone)
- Equivalent analgesia to oxycodone CR
- Naloxone component reduces opioid induced constipation
- NNT = 4 for existing opioid induced constipation
- NNT = 14 for people not selected for constipation (aperients often still required, especially for pre-existing constipation)
- Oral naloxone component has low systemic bioavailability and decreases GI opioid effects
- Maximum dose 80mg/ 40mg daily, if above this then the 40mg naloxone likely to reach systemic circulation
- Decreased dose in mild hepatic impairment or CrCl < 60ml/min
- Naloxone component may deter injected or intranasal use
- Buprenorphine patch (Norspan) and Fentanyl Patch (Durogesic) patch
- Not suitable for acute pain
- Patches not suitable for patients that are very slim or having high fevers
- Buprenorphine patches are option for people who require low doses of opioids for persistent pain
- Given as weekly patch
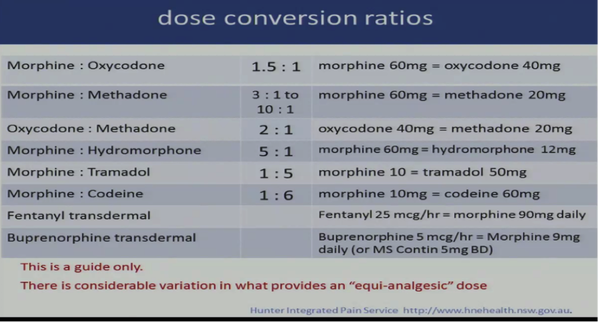
- Buprenorphine patch 5mcg/hour – MS Contin 5mg BD
- Largest patch available in Australia 20mcg/hour
- Fentanyl patches are an option for stable severe chornic pain and established opioid needs
- Start 12mcg/hr patch applied every 72hrs
- Fentanyl patch 25mcg/hour = Morphine 90mg orally daily
- Not appropriate for opioid naive patients – risk of fatal opioid overdose
- Street value – residual fentanyl
- Use co-anagesics + adjuvants for neuropathic pain
- anti-epileptic drugs include valproate 200mg OD - BD, increasing as tolerated to max 1500mg daily in divided dose
- Gabapentin and pregabalin
- pregabalin 75mg/ gabapentin 100mg
- Α2δ subunit of calcium channels: brain and dorsal horn
- Good evidence: neuropathic pain, fibromyalgia
- Some evidence: low back pain with radiculopathy
- No evidence: no specific low back pain
- TCAs - amitriptyline 10mg noce, increasing every 7 days
- SNRI: duloxetine 30mg daily
- Other options
- Baclofen for spasticity
- Palliative for malignant pain: regional blocks,
- Radiofrequency ablation of spinal nerves
- Long term epidural infusions (<2months)
- Coeliac plexus ablation with phenol injections (mainly for pancreatic cancer)
- Deep brain stimulators or thalamic ablations (extreme stuff)
- Trigeminal ablations: for severe trigeminal neuralgia