Question 1
Which atrial septum defect is commonly associated with endocardial cushion defects in down’s syndrome?
(A) Patent Foramen ovale
(B) Ostium Primum
(C) Ostium Secundum
(D) Sinus Vensous defect
(E) Cor-triatrium
B: Down’s syndrome is associated with endocardial cushion defects, meaning that the middle of the heart does not form properly. As such, these patients tend to have primum defects, rather than secundum defects. RPA lectures 2015
Question 2
What is the most common type of atrial septal defect?
(A) Patent Foramen ovale
(B) Ostium Primum
(C) Ostium Secundum
(D) Sinus Vensous defect
(E) Cor-triatrium
C: An ostium secundum defect occurs in the middle of the interatrial septa. RPA lectures 2015
Question 3
A 26 year old patient is taken to the cardiac catheter laboratory by an overzealous cardiologist to investigate causes for his paradoxical embolism. With regards to right heart catheterisation, in which anatomical area would you find the lowest oxygen saturations?
(A) Inferior Vena Cava
(B) Superior Vena Cava
(C) Right Atrium
(D) Right Ventricle
(E) Pulmonary Vein
B: Superior vena cava, simply because blood is going to a more metabolically active area leading to increased oxygen extraction. Circulation 2008; 118:e714.
Question 4
A 34 year old male with down’s syndrome presents cyanosed, short of breath and worsening peripheral oedema and abdominal girth. He has had multiple respiratory tract infections in the past. He is fatigued. On examination he has evidence of pulmonary hypertension with a tricuspid regurgitation murmur, a prominent ‘a’ wave and right ventricular heave. In addition there is a pulsatile liver and evidence of ascites. ECG reveals atrial fibrillation with evidence of RV strain. Echocardiography reveals a dilated right ventricule with severe tricuspid regurgitation and an estimated RV-RA pressure of 70 mm Hg. There is evidence of an ostium primum defect. Right heart catheterisation reveals a shunt fraction Qp:Qs of 0.8 and a pulmonary vascular resistance of 10. What is the correct management of this patient?
(A) He should have open closure of his ostium primum defect
(B) He should have percutaneous closure of his ostium primum defect
(C) He should be medically managed
(D) He should have endocardial pacing if he develops a class 1 indication for pacing
(E) He should routinely require therapeutic anticoagulation
C: He has an atrial septal defect with Eisenmenger physiology where there is shunt reversal and pulmonary vascular resistance > 7 or 8 WU. Management of this syndrome is medical. There is no class 1 evidence to support the use of therapeutic anticoagulation in this case.
Question 5
A 34 year old male presents with pleuritic chest pain which is relieved upon sitting forward. He was previously sick with an upper respiratory tract infection. Examination reveals a haemodynamically stable well looking gentleman. There is no pulses paradoxus. Auscultation reveals no crackles but there is a pericardial rub with soft heart sounds. ECG shows wide-spread ST elevation and PR depression. He has no other co-morbidities. What is the optimal management for this individual?
(A) Colchicine
(B) High dose NSAIDS
(C) Corticosteroids
(D) Colchicine + high dose NSAIDS
(E) Observation
D: Combination treatment with high dose NSAIDS and colchicine - an inhibitor of microtubule formation, is the favoured treatment regime. It decreases persistent symptoms as well as decreasing recurrence rates compared to single agent alone. Corticosteroids should be avoided when they can as they increase the risk of recurrence. Note that small pericardial effusions in acute pericarditis occurs in 66% of patients, mostly they are small and of minimal significance. Recurrent pericarditis should be treated with repeat courses of NSAIDS and colchicine, with glucocorticoids only reserved for the true refractory cases. N Engl J Med 2014; 371:2410-2416.
Question 6
Which of the following is NOT an indication for closure of an atrial septal defect
(A) Right ventricular dilatation
(B) Qp:Qs >1.5
(C) ASD defect 7mm
(D) Stroke from paradoxical embolism
C: The ASD defect has to be >10mm if asymptomatic to warrant closure. Small defects should be followed up. All the other options are indications. Note that Eisenmenger physiology is a contraindication to closure of the defect. RPA lectures 2015
Question 7
Which of the following is NOT associated with a tetralogy of fallot
(A) Overriding aorta
(B) Ventricular septal defect
(C) Hypertrophied Right Ventricle
(D) Atrial septal defect
(E) Anteriorly deviated septum with narrowing of the RV tract
D: The primary pathology of tetralogy of fallot seems to be the anteriorly deviated septum. This causes a VSD, narrowed RVOT, an overriding aorta and RV hypertrophy. RPA lectures 2015
Question 8
What is the most common complication seen in patients who have had their tetralogy of fallot repaired?
(A) Pulmonary stenosis
(B) Pulmonary regurgitation
(C) Right heart failure
(D) Arrhythmia
(E) Mitral regurgitation
B: All the following apart from E are potential complications, but based on the surgery type the most common complication is free pulmonary regurgitation. The biggest cause of death post repair is with pulmonary regurgitation. Many of these patients may require a bioprosthetic pulmonary valve replacement. RPA lecture 2015-12-23
Question 9
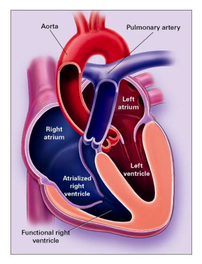
What is FALSE regarding ebsteins anomoly?
(A) A portion of the right ventricle is 'atrialised'
(B) 80% association with atrial septal defect
(C) 40% association with ventricular septal defect
(D) 20% associated with an accessory conduction pathway leading to ventricular pre-excitation
(E) Haemodynamic compromise results from increased right atrial pressures and right to left interatrial shunting
C: Ebsteins anomoly results from an abnormality of the tricuspid valve such that the septal leaflets and often the posterior leaflets are displaced into the right ventricle and the anterior leaflet is usually malformed, excessively large, and abnormally attached or adherent to the right ventricular free wall. Therefore a portion of the right ventricle lies within the atrial side of the tricuspid valve and the remaining right ventricle is small. N Engl J Med 2000; 342:334-342 (see below for picture)
Question 10
With regards to transposition of the great arteries, what is NOT a management strategy?
(A) Prostaglandin E infusion
(B) Oxygen
(C) Arterial switch procedure
(D) Atrial switch procedure
(E) none of the above
E: Prostaglandin E keeps the PDA open, thus allowing intracardiac mixing. Oxygen decreases pulmonary vascular resistance. Arterial switch procedure and atrial switch procedure are surgical corrective procedures that can be performed to correct the congenital defect. N Engl J Med 2000; 342:334-342
Question 11
What percentage of ventricular septal defects in childhood close in adulthood?
(A) 20%
(B) 40%
(C) 60%
(D) 80%
(E) 90%
E: The most common type of ventricular septal defect is the membranous type (70%), followed by muscular. N Engl J Med 2000; 342:334-342
Question 12
What is NOT the correct paring of congenital heart defects?
(A) Ostium primum defect AND mitral regurgitation
(B) Ostium secundum defect AND mitral valve prolapse
(C) Sinus venosus defect AND partial anomolous venous return of the pulmonary veins
(D) Sinus venosus defect AND down's syndrome
(E) Ebsteins anomoly AND tricuspid regurgitation
D: Ostium primum defects are associated with down's syndrome N Engl J Med 2000; 342:334-342, RPA Course 2015
Question 13
What is CORRECT about the anatomy of a patent ductus arteriosus
(A) It connects the ascending aorta to the right main pulmonary artery
(B) It connects the descending aorta to the left main pulmonary artery
(C) It connects the ascending aorta to the left main pulmonary artery
(D) It connects the ascending aorta to the left main pulmonary artery
(E) It connects the ascending aorta to the main pulmonary trunk.
B: N Engl J Med 2000; 342:334-342
Question 14
Which of the following has the greatest mortality benefit in a patient with heart failure and reduced ejection fraction?
(A) ACE-I
(B) Angiotensin Receptor blocker
(C) Mineralocorticoid receptor
(D) Digoxin
(E) Beta-blocker
E: PEP2014
Question 15: EMQ on Lipid targets as per eTG
(A) 2mM
(B) 2.5mM
(C) 3mM
(D) 1mM
(E) 4mM
(F) 10mM
(G) 15mM
What level should the LDL-C concentration be lowered to as a target in primary prevention?
A
What level should total cholesterol be targeted below in primary prevention studies?
E
What level should HDL-C concentration be raised above in primary prevention studies?
D
Question 16
Alcohol use may cause an elevation in which of the following lipids?
(A) Triglycerides
(B) LDL
(C) HDL
(D) IDL
(E) Chylomicrons
A and/ or C: eTG 2012
Question 17
Hypothyroidism causes an elevation in which of the following lipids?
(A) Triglycerides
(B) LDL
(C) HDL
(D) IDL
(E) Chylomicrons
B: Additional secondary causes of increased LDL-C include nephrotic syndrome, cholestasis, anorexia nervosa. Triglycerides are elevated in type 2 diabetes (associated with decreased HDL) and smoking. Oestrogen use also elevates triglycerides and may also increase HDL - eTG 2012
Question 18
According to the Australian Therapeutic guidelines, what is the most appropriate dietary modification that reduces LDL-C?
(A) Reducing saturated fats and trans fats
(B) Replacing saturated fats with monosaturated fats
(C) Replacing saturated fats with polyunsaturated fats
(D) Increasing intake of soluble fibre
(E) Introducing plant sterol containing milk, margarine or cheese products
E: This is the most effective dieatary intervention, leading to an approximate reduction in LDL-C by 10 - 15%
Question 19
Which of the following is NOT recognised as a non-pharmacological strategy to decrease the impact of orthostatic hypotension?
(A) Avoiding hot baths
(B) Increasing fluid intake
(C) Increasing salt intake
(D) Wearing waist height compression stockings
(E) Prolonged standing exercises
E: ETG 2016
Question 20
What is the mechanism of action of ezetimibe, which has been shown in the IMPROVE-IT trial to reduce LDL cholesterol and cardiovascular outcomes in combination with simvastatin over and beyond the effect of the statin itself?
(A) It inhibits reabsorption of triglycerides via the fatty acid transporter on the apical brush border membrane of the enterocytes
(B) Ezetimibe targets the Niemann–Pick C1–like 1 (NPC1L1) protein, thereby reducing absorption of cholesterol from the intestine
(C) It reduces the conversion of acetyl CoA to malonyl CoA
(D) It uncouples fatty acid beta-oxidation processes in the mitochondria
(E) It reduces cholesteral absorption from the intestine by disrupting micelle formation and cholecystokinin induced gall bladder contraction
B: Polymorphisms affecting NPC1L1 are associated with both lower levels of LDL cholesterol and a lower risk of cardiovascular events. N Engl J Med 2015; 372:2387-2397
Question 21
Which of the following is a physical sign of severe mitral stenosis
(A) Heaving apex beat
(B) Atrial Fibrillation
(C) Short S2 - Opening snap time interval
(D) S3
(E) Split S1
C: Other signs of severity include a tapping apex beat, signs of pulmonary hypertension, signs of left heart failure, pre-systolic accentuation of the diastolic murmur, length of the diastolic murmur. The murmur of mitral stenosis is best heard with the bell of the stethoscope as it is a low pitch rumble, at the apex in the left lateral position, in full expiration.
Question 22
A 67 year old male presents with abdominal pain, recurrent wheezing and facial flushing. He has fluctuating blood pressure and secretory diarrhoea. CT abdomen reveals multiple lesions on the liver and luminal thickening over the appendix. Plasma is positive for chromogranin A. Urinary 5-HIAA is positive. What would be the most likely finding on cardiac auscultation.
(A) A harsh ejection systolic murmur over the left sternal edge that accentuates from supine to standing
(B) An ejection systolic murmur over the aortic region radiating to the carotids
(C) A pan-systolic murmur over the left sternal edge that accentuates after 2 minutes of isometric grip exercise
(D) A low rumbling mid diastolic murmur over the left sternal edge, which is accentuated by inspiration
(E) A pan-systolic murmur over the cardiac apex radiating to the axilla, accentuated by expiration
D: This patient has carcinoid syndrome, which characteristically has right sided murmurs. The only right sided murmur hear is option D, which is the associated murmur of tricuspid stenosis. Typically, right sided murmurs accentuate with inspiration as a result of increased venous return and increased right sided flows.
EMQ
Match the following valvular pathologies to the associated auscultatory findings on cardiac clinical examination
(A) Mitral Stenosis
(B) Mitral Regurgitation
(C) Mitral Prolapse
(D) Hypertrophic Obstructive Cardiomyopathy
(E) Atrial Septal Defect
(F) Ventricular Septal Defect
(G) Aortic Stenosis
(H) Aortic Sclerosis
(I) Aortic Regurgitation
A harsh ejection systolic murmur over the 2nd intercostal space, left sternal edge with normal second heart sound and no radiation to the carotids
H: Aortic sclerosis sounds like aortic stenosis however there is an absence of other peripheral signs. Echocardiography will reveal thickened valvular cusps without a haemodynamically significant gradient across the aortic valve.
A harsh ejection systolic murmur heard best over the apex, high pitch in nature, radiating to the axilla, with a soft second heart sound
G: This is aortic stenosis with the gallavardin phenomenon, where high frequency components of the murmur radiate to the apex and axilla. The soft second heart sound is also a clue, as this does not occur in mitral regurgitiaton.
A pansystolic murmur heard best over the apex accentuated by expiration and radiating to the axilla, with a third heart sound heard best in expiration
B: This is the classic murmur of mitral regurgitation. Signs of severity include signs of left ventricular failure, signs of right ventricular failure, a narrow pulse pressure, an apical thrill, a laterally displaced and thrusting apex beat and a third heart sound. Atrial fibrillation may co-exist secondary to left atrial enlargement. Acute mitral regurgitation is a surgical emergency and is most commonly a result of infarction.
A fixed and wide split second heart sound with a soft ejection systolic murmur over the pulmonary region
E: There is no respiratory variation in the second heart sound due to equalisation of pressures through the atria. That is, with increased venous return, increases in right atrial pressure reduces the shunt from the left atrium. The split is wider because there is a left to right shunt through the septaldefect. An ostium secundum defect is the most common type and can be fixed through percutaneous devices. Other defects include ostium primum defects which are associated with endocardial cushion defects, and sinus venosum defects which is associated with anomalous pulmonary venous drainage
A high-pitched, decrescendo diastolic murmur obscuring the second heart sound, heard best over the left sternal edge in expiration.
I: This is the murmur of aortic regurgitation. This may co-occur with a ventricular septal defect, commonly involving the anterior leaflet of the aortic valve.
A harsh ejection systolic murmur heard best over the left sternal edge, accentuated with expiration and decreased by isometric hand grip exercise manoeuvre
D: Hypertrophic obstructive cardiomyopathy causes dynamic left ventricular outflow tract obstruction, whereby the obstruction increases with decreased left ventricular volume, commonly through preload diminishing manoeuvres. Any manoeuvre which increases preload will increase ventricular volume and thus diminish the outflow gradient and the intensity of the murmur. The murmur may also be associated with mitral regurgitation through the mechanism of systolic anterior motion.
Question 23
A 46 year old male is admitted under the gastroenterology team with massive ascites and peripheral oedema. On clinical examination there is evidence of shifting dullness, pitting oedema, bilateral pleural effusions, ‘v’ waves and a pan-systolic murmur accentuated by inspiration over the left sternal edge, 5th intercostal space. In addition, cardiac auscultation reveals an early diastolic murmur over the left sternal edge, 2nd intercostal space, again accentuated by inspiration. There is also a loud pan-systolic murmur over the cardiac apex associated with a thrill. This murmur radiates to the axilla and is accentuated by expiration. There is a left ventricular third heart sound. The apex beat is displaced inferior-laterally and is thrusting in nature. What is the most dominant lesion and what are the associated valvular pathologies revealed by cardiac examination?
(A) Tricuspid regurgitation, no other lesion
(B) Tricuspid regurgitation, with Pulmonary Stenosis
(C) Mitral regurgitation, with pulmonary regurgitation and Tricuspid stenosis
(D) Mitral regurgitation, with pulmonary regurgitation and Tricuspid regurgitation
(E) Tricuspid stenosis, with tricuspid regurgitation
D: Mitral regurgitation is the dominant murmur given the thrill, the displaced apex beat and the left ventricular third heart sound. The diastolic murmur is that of functional pulmonary regurgitation (Graham-steel murmur) and there is associated severe tricuspid regurgitation with ‘v’ waves, ascites and pitting oedema.
Question 24
Which of the following is a sign of severity of aortic regurgitation?
(A) A mid-diastolic rumbling murmur heard best with the bell of the stethoscope
(B) An ejection systolic murmur over the aortic region
(C) A soft first heart sound
(D) A short diastolic murmur
(E) A heaving apex beat
A: This is the Austin flint murmur, caused by the regurgitant jet striking the mitral valve leaflet during LA to LV flow in diastole, mimicking mitral stenosis. Co-existent aortic stenosis is common, and an ejection systolic murmur over the aortic region may represent a flow murmur when the left ventricle ejects the regurgitant volume.
Question 25
The third sound corresponds to which part of the cardiac cycle?
(A) Pressure-volume change during systole
(B) Isovolumetric contraction
(C) Isovolumetric relaxation
(D) Pressure volume change during diastole
(E) Atrial systole
D: Pressure volume changes occur during systole and diastole. During systole and diastole, there is a short period of time corresponding to increased pressure/ decreased pressure without volume change, known as isovolumetric relaxation and contraction respectively. S3 corresponds to rapid ventricular filling, which occurs during diastole. S4 corresponds to the atrial kick against a non-compliant left ventricle, and it does not occur in atrial fibrillation.
Question 26
Which of the following is a feature of cardiac myocyte muscle?
(A)
With regards to transposition of the great arteries, what is NOT a management strategy?
(A) Prostaglandin E infusion
(B) Oxygen
(C) Arterial switch procedure
(D) Atrial switch procedure
(E) none of the above
E: Prostaglandin E keeps the PDA open, thus allowing intracardiac mixing. Oxygen decreases pulmonary vascular resistance. Arterial switch procedure and atrial switch procedure are surgical corrective procedures that can be performed to correct the congenital defect. N Engl J Med 2000; 342:334-342
Question 11
What percentage of ventricular septal defects in childhood close in adulthood?
(A) 20%
(B) 40%
(C) 60%
(D) 80%
(E) 90%
E: The most common type of ventricular septal defect is the membranous type (70%), followed by muscular. N Engl J Med 2000; 342:334-342
Question 12
What is NOT the correct paring of congenital heart defects?
(A) Ostium primum defect AND mitral regurgitation
(B) Ostium secundum defect AND mitral valve prolapse
(C) Sinus venosus defect AND partial anomolous venous return of the pulmonary veins
(D) Sinus venosus defect AND down's syndrome
(E) Ebsteins anomoly AND tricuspid regurgitation
D: Ostium primum defects are associated with down's syndrome N Engl J Med 2000; 342:334-342, RPA Course 2015
Question 13
What is CORRECT about the anatomy of a patent ductus arteriosus
(A) It connects the ascending aorta to the right main pulmonary artery
(B) It connects the descending aorta to the left main pulmonary artery
(C) It connects the ascending aorta to the left main pulmonary artery
(D) It connects the ascending aorta to the left main pulmonary artery
(E) It connects the ascending aorta to the main pulmonary trunk.
B: N Engl J Med 2000; 342:334-342
Question 14
Which of the following has the greatest mortality benefit in a patient with heart failure and reduced ejection fraction?
(A) ACE-I
(B) Angiotensin Receptor blocker
(C) Mineralocorticoid receptor
(D) Digoxin
(E) Beta-blocker
E: PEP2014
Question 15: EMQ on Lipid targets as per eTG
(A) 2mM
(B) 2.5mM
(C) 3mM
(D) 1mM
(E) 4mM
(F) 10mM
(G) 15mM
What level should the LDL-C concentration be lowered to as a target in primary prevention?
A
What level should total cholesterol be targeted below in primary prevention studies?
E
What level should HDL-C concentration be raised above in primary prevention studies?
D
Question 16
Alcohol use may cause an elevation in which of the following lipids?
(A) Triglycerides
(B) LDL
(C) HDL
(D) IDL
(E) Chylomicrons
A and/ or C: eTG 2012
Question 17
Hypothyroidism causes an elevation in which of the following lipids?
(A) Triglycerides
(B) LDL
(C) HDL
(D) IDL
(E) Chylomicrons
B: Additional secondary causes of increased LDL-C include nephrotic syndrome, cholestasis, anorexia nervosa. Triglycerides are elevated in type 2 diabetes (associated with decreased HDL) and smoking. Oestrogen use also elevates triglycerides and may also increase HDL - eTG 2012
Question 18
According to the Australian Therapeutic guidelines, what is the most appropriate dietary modification that reduces LDL-C?
(A) Reducing saturated fats and trans fats
(B) Replacing saturated fats with monosaturated fats
(C) Replacing saturated fats with polyunsaturated fats
(D) Increasing intake of soluble fibre
(E) Introducing plant sterol containing milk, margarine or cheese products
E: This is the most effective dieatary intervention, leading to an approximate reduction in LDL-C by 10 - 15%
Question 19
Which of the following is NOT recognised as a non-pharmacological strategy to decrease the impact of orthostatic hypotension?
(A) Avoiding hot baths
(B) Increasing fluid intake
(C) Increasing salt intake
(D) Wearing waist height compression stockings
(E) Prolonged standing exercises
E: ETG 2016
Question 20
What is the mechanism of action of ezetimibe, which has been shown in the IMPROVE-IT trial to reduce LDL cholesterol and cardiovascular outcomes in combination with simvastatin over and beyond the effect of the statin itself?
(A) It inhibits reabsorption of triglycerides via the fatty acid transporter on the apical brush border membrane of the enterocytes
(B) Ezetimibe targets the Niemann–Pick C1–like 1 (NPC1L1) protein, thereby reducing absorption of cholesterol from the intestine
(C) It reduces the conversion of acetyl CoA to malonyl CoA
(D) It uncouples fatty acid beta-oxidation processes in the mitochondria
(E) It reduces cholesteral absorption from the intestine by disrupting micelle formation and cholecystokinin induced gall bladder contraction
B: Polymorphisms affecting NPC1L1 are associated with both lower levels of LDL cholesterol and a lower risk of cardiovascular events. N Engl J Med 2015; 372:2387-2397
Question 21
Which of the following is a physical sign of severe mitral stenosis
(A) Heaving apex beat
(B) Atrial Fibrillation
(C) Short S2 - Opening snap time interval
(D) S3
(E) Split S1
C: Other signs of severity include a tapping apex beat, signs of pulmonary hypertension, signs of left heart failure, pre-systolic accentuation of the diastolic murmur, length of the diastolic murmur. The murmur of mitral stenosis is best heard with the bell of the stethoscope as it is a low pitch rumble, at the apex in the left lateral position, in full expiration.
Question 22
A 67 year old male presents with abdominal pain, recurrent wheezing and facial flushing. He has fluctuating blood pressure and secretory diarrhoea. CT abdomen reveals multiple lesions on the liver and luminal thickening over the appendix. Plasma is positive for chromogranin A. Urinary 5-HIAA is positive. What would be the most likely finding on cardiac auscultation.
(A) A harsh ejection systolic murmur over the left sternal edge that accentuates from supine to standing
(B) An ejection systolic murmur over the aortic region radiating to the carotids
(C) A pan-systolic murmur over the left sternal edge that accentuates after 2 minutes of isometric grip exercise
(D) A low rumbling mid diastolic murmur over the left sternal edge, which is accentuated by inspiration
(E) A pan-systolic murmur over the cardiac apex radiating to the axilla, accentuated by expiration
D: This patient has carcinoid syndrome, which characteristically has right sided murmurs. The only right sided murmur hear is option D, which is the associated murmur of tricuspid stenosis. Typically, right sided murmurs accentuate with inspiration as a result of increased venous return and increased right sided flows.
EMQ
Match the following valvular pathologies to the associated auscultatory findings on cardiac clinical examination
(A) Mitral Stenosis
(B) Mitral Regurgitation
(C) Mitral Prolapse
(D) Hypertrophic Obstructive Cardiomyopathy
(E) Atrial Septal Defect
(F) Ventricular Septal Defect
(G) Aortic Stenosis
(H) Aortic Sclerosis
(I) Aortic Regurgitation
A harsh ejection systolic murmur over the 2nd intercostal space, left sternal edge with normal second heart sound and no radiation to the carotids
H: Aortic sclerosis sounds like aortic stenosis however there is an absence of other peripheral signs. Echocardiography will reveal thickened valvular cusps without a haemodynamically significant gradient across the aortic valve.
A harsh ejection systolic murmur heard best over the apex, high pitch in nature, radiating to the axilla, with a soft second heart sound
G: This is aortic stenosis with the gallavardin phenomenon, where high frequency components of the murmur radiate to the apex and axilla. The soft second heart sound is also a clue, as this does not occur in mitral regurgitiaton.
A pansystolic murmur heard best over the apex accentuated by expiration and radiating to the axilla, with a third heart sound heard best in expiration
B: This is the classic murmur of mitral regurgitation. Signs of severity include signs of left ventricular failure, signs of right ventricular failure, a narrow pulse pressure, an apical thrill, a laterally displaced and thrusting apex beat and a third heart sound. Atrial fibrillation may co-exist secondary to left atrial enlargement. Acute mitral regurgitation is a surgical emergency and is most commonly a result of infarction.
A fixed and wide split second heart sound with a soft ejection systolic murmur over the pulmonary region
E: There is no respiratory variation in the second heart sound due to equalisation of pressures through the atria. That is, with increased venous return, increases in right atrial pressure reduces the shunt from the left atrium. The split is wider because there is a left to right shunt through the septaldefect. An ostium secundum defect is the most common type and can be fixed through percutaneous devices. Other defects include ostium primum defects which are associated with endocardial cushion defects, and sinus venosum defects which is associated with anomalous pulmonary venous drainage
A high-pitched, decrescendo diastolic murmur obscuring the second heart sound, heard best over the left sternal edge in expiration.
I: This is the murmur of aortic regurgitation. This may co-occur with a ventricular septal defect, commonly involving the anterior leaflet of the aortic valve.
A harsh ejection systolic murmur heard best over the left sternal edge, accentuated with expiration and decreased by isometric hand grip exercise manoeuvre
D: Hypertrophic obstructive cardiomyopathy causes dynamic left ventricular outflow tract obstruction, whereby the obstruction increases with decreased left ventricular volume, commonly through preload diminishing manoeuvres. Any manoeuvre which increases preload will increase ventricular volume and thus diminish the outflow gradient and the intensity of the murmur. The murmur may also be associated with mitral regurgitation through the mechanism of systolic anterior motion.
Question 23
A 46 year old male is admitted under the gastroenterology team with massive ascites and peripheral oedema. On clinical examination there is evidence of shifting dullness, pitting oedema, bilateral pleural effusions, ‘v’ waves and a pan-systolic murmur accentuated by inspiration over the left sternal edge, 5th intercostal space. In addition, cardiac auscultation reveals an early diastolic murmur over the left sternal edge, 2nd intercostal space, again accentuated by inspiration. There is also a loud pan-systolic murmur over the cardiac apex associated with a thrill. This murmur radiates to the axilla and is accentuated by expiration. There is a left ventricular third heart sound. The apex beat is displaced inferior-laterally and is thrusting in nature. What is the most dominant lesion and what are the associated valvular pathologies revealed by cardiac examination?
(A) Tricuspid regurgitation, no other lesion
(B) Tricuspid regurgitation, with Pulmonary Stenosis
(C) Mitral regurgitation, with pulmonary regurgitation and Tricuspid stenosis
(D) Mitral regurgitation, with pulmonary regurgitation and Tricuspid regurgitation
(E) Tricuspid stenosis, with tricuspid regurgitation
D: Mitral regurgitation is the dominant murmur given the thrill, the displaced apex beat and the left ventricular third heart sound. The diastolic murmur is that of functional pulmonary regurgitation (Graham-steel murmur) and there is associated severe tricuspid regurgitation with ‘v’ waves, ascites and pitting oedema.
Question 24
Which of the following is a sign of severity of aortic regurgitation?
(A) A mid-diastolic rumbling murmur heard best with the bell of the stethoscope
(B) An ejection systolic murmur over the aortic region
(C) A soft first heart sound
(D) A short diastolic murmur
(E) A heaving apex beat
A: This is the Austin flint murmur, caused by the regurgitant jet striking the mitral valve leaflet during LA to LV flow in diastole, mimicking mitral stenosis. Co-existent aortic stenosis is common, and an ejection systolic murmur over the aortic region may represent a flow murmur when the left ventricle ejects the regurgitant volume.
Question 25
The third sound corresponds to which part of the cardiac cycle?
(A) Pressure-volume change during systole
(B) Isovolumetric contraction
(C) Isovolumetric relaxation
(D) Pressure volume change during diastole
(E) Atrial systole
D: Pressure volume changes occur during systole and diastole. During systole and diastole, there is a short period of time corresponding to increased pressure/ decreased pressure without volume change, known as isovolumetric relaxation and contraction respectively. S3 corresponds to rapid ventricular filling, which occurs during diastole. S4 corresponds to the atrial kick against a non-compliant left ventricle, and it does not occur in atrial fibrillation.
Question 26
Which of the following is a feature of cardiac myocyte muscle?
(A)