Lung Transplantation
History
- Pre-Transplantation work-up
- 16-65 with a life expectancy <2 years, non smoking 1 year. In US >19% of pts >65 who have lung Tx, therefore strong argument for functional age rather than chronological age
- Contra-indications include: (1) recent malignancy (other than nonmelanoma skin cancer); (2) active infection with hepatitis B or C virus associated with histologic evidence of significant liver damage; (3) active or recent cigarette smoking, drug abuse, or alcohol abuse; (4) severe psychiatric illness; (5) repeated noncompliance with medical care; (6) absence of a consistent and reliable social support network
- Prior pleurodesis is associated with an increased risk of intraoperative bleeding, particularly when cardiopulmonary bypass is used, but is not a contraindication to transplantation
- Cardio-pulmonary function test: Angiography, Echocardiography, CT Chest, Formal Respiratory function tests
- Psychosocial factors (see liver, renal transplant for discussion)
- Lung allocation score calculated from a priority algorithm including matching for ABO compatibility, lung size, type and severity of lung disease
- Uses Cox proportional hazard models to calculate 1-year survival without and with transplantation
- raw Lung allocation score = net transplant benefit (one year survival with transplant − one year survival without transplant) minus medical urgency (one year survival without transplant)
- The lung allocation score is made on a scale of 0 - 100 after being normalised, higher scores imply greater need
- Disease specific criterion for consideration of transplantation
- COPD: (1) BODE 7 - 10 OR one of (1) hospitalisation with T2RF CO2 >50 (2) Pulm HTN/ cor pulmonale despite O2 (3) FEV1 <20% AND either DLCO <20% or homogenous distribution emphysema
- IPF: Histologic or radiographic evidence of UIP and any of the following (1) A DlCO < 39% predicted (2) A 10% or greater decrement in FVC during 6 mo of follow-up (3) A decrease in pulse oximetry below 88% during a 6MW (4) Honeycombing on HRCT (fibrosis score of > 2)
- Cystic Fibrosis: FEV1 < 30 % predicted, or rapidly declining lung function if FEV1 > 30 % predicted (women and patients < 18 yr of age have a poorer prognosis; consider earlier listing) and/or any of the following (1) Increasing oxygen requirements (2) Hypercapnia and (3) Pulmonary hypertension
- Idiopathic pulmonary arterial hypertension: (1) Persistent NYHA class III or IV on maximal medical therapy (2) Low (350 m) or declining 6MWT (3) Failing therapy with intravenous epoprostenol, or equivalent. (4) Cardiac index of < 2 L/min/m2 (5) Right atrial pressure > 15 mm Hg
- Surgical Procedure
- Single lung transplants and bilateral lung transplants are performed (97%) much more commonly than combined heart-lung transplants (3%), which is now reserved for patients with Eisenmenger syndrome with surgically uncorrectable cardiac defects
- Heart lung Tx may be performed for idiopathic pulmonary arterial hypertension, but now recognised that RV can recover after decreases in pulmonary arterial pressure
- BLT is the exclusive procedure for patients with CF/ bronchiectesis because of concerns related to leaving a chronically infected lung in place with SLT
- Complications
- Primary graft dysfunction: acute allograft injury characterized by development of noncardiogenic pulmonary edema within 72 hours of transplantation in the absence of identifiable secondary causes - probably related to ischaemic reperfusion injury. Rx supportive with lung protective ventilatory strategies. Note it is a leading cause of death in the perioperative period
- Airway dysfunction: during the operation no attempt is made to establish systemic flow through bronchial arteries, therefore donor bronchus must derive all its blood flow through retrograde flow via the venous system --> airways at risk of ischaemic injury. Can lead to severe airway dehiscence. Devitalised areas can be a nidus for fungal super-infection
- Bronchial stenosis as a delayed injury pattern to initial ischaemia
- Infection: leading cause of mortality. Bronchial pneumonia peaks first month of Tx, Pseudomonas is most common organism, followed by S. aureus. CMV very common even with prophylaxis, one third develop CMV disease within first year post Tx. Sero-discordant pairs are at highest risk
- CMV disease: whist rising viral titre usually signifies disease, correlation with tissue specific disease not the best, therefore to be absolutely sure need Bx or BAL to show inclusion bodies. Universal prophylaxis with valganciclovir is important. Consensus guidelines recommend a minimum of 6 months of prophylaxis for donor-positive/recipient-negative patients and 3 to 6 months for recipient-positive patients. NB RCT recently showed 12 months prophylaxis superior to 6 months.
- Aspergillus: can involve airway, lung parenchyma or extra-pulmonary invasion. airway infections usually asymptomatic, picked up on surveillance bronchoscopy. Invasive aspergillus is common. Rx with voriconazole, second line option is echinocandins and amphotericin. Mortality of invasive aspergillus approaching 60%
- Rejection: 50% acute cellular rejection in first yr. Sx include fever, dyspnoea, cough but can be asymptomatic. Biopsy will show perivascular lymphocytic infiltrate. Rx with 3/7 course of methylpred, usually with resolution
- Bronchiolitis Obliterans Syndrome (BOS): Most common cause of chronic allograft dysfunction. Fibroproliferative process that obliterates the smaller airways, and eventually the larger airways. FEV1 is used as a surrogate marker as histology difficult to obtain. 50% develop BOS in 5 years, 75% in 10 years. Defined as an unexplained decline in FEV1 by 20%. Difficult to Rx
- Management:
- Surveillance: Symptoms, regular PFTs (↓FEV1) → CXR, bronchoscopy
- Immunosuppression: Similar to other transplants. Have induction regimes (deplete the recipient immune system in the immediate post-transplant period to decrease early interaction between the recipient immune cells and donor allograft antigens because there is concern that early alloreactivity not only leads to increased acute rejection but to chronic low level inflammation)
- Induction regimes include OKT3 (murine monoclonal antibody directed against the epsilon chain of the T cell receptor–CD3 complex, resulting in prevention of T cell activation and depletion of circulating T cells with relative sparing of T regulatory cells - initially causes activation and cytokine release syndrome), Antithymocyte globulin is a polyclonal antibody nonspecifically directed at lymphocytes produced by inoculating animals with human thymocytes. Basiliximab - against IL2R (CD25). Basiliximab is currently approved for dosing 20 mg on the first and fourth days after transplant, half life 13 days, dosing schedule results in 30 days of IL2R saturation.
- Malignancy: 3-4x fold in skin cancers, PTLD, Kaposis, bowel cancer
- Scar with normal sounds on same side
- Infection? Sputum
- End-inspiratory pops/squeaks (can be bronchiolitis obliterans or bronchiectasis)
- Cushingoid
- Systemic changes from underlying disease
- Cor Pulmonale
- 75% @ 1yr, 50% @ 5yrs
- 10% die on waiting list, much higher if IPF< PAH, CF than COPD
- Main cause of death is rejection, followed by infections (CMV and non
Obstructive Sleep Apnoea and other sleep related issues
General
Obesity Hypoventilation Syndrome
Restless Leg Syndrome
Differential diagnosis for daytime somnolence
Idiopathic Hypersomnolence
Narcolepsy
- Repetitive collapse of the upper airway during sleep
- Defined as Apnoea-Hypopnoea Index (AHI) =>5 per hour
- Apnoea = complete cessation of ventilation for > 10 seconds
- Hypopnoea = partial reduction of ventilation
- Classification according to AHI: (1) 5-15 mild (2) 15-30 mod and (3) >30 severe
- Snoring is not a key component of OSA.
- Poorer quality of life eg leads to greater divorces
- untreated OSA --> significant perioperative risk of respiratory failure. For orthopaedic surgery there is a statistically increased risk for PE, ARDS, aspiration and intubation
- Snoring
- Apnoeas and sleep arousals
- Consider central apnoea in Pts with absence of significant snoring, but note that a clear association does not exist
- Excessive daytime somnolence, fatigue, depression, poor concentration
- Early morning headaches
- Epworth sleepiness scale
- Can you remain awake to watch news? Movie?
- Do you feel safe to drive? If no
- Duration of trip (>2 hours)
- Prior shift duration (< 5 hours)
- Shift work
- Time of drowsiness
- Cause of secondary hypertension
- Obesity
- Oropharangeal crowding: short mandible, soft tissues, enlarged tonsils
- EtOH consumption
- Smoking
- Medications – e.g hypnotics that may have been prescribed for poor sleeping but aggravate OSA
- Cardiovascular disease: HTN, IHD, CVA, Arrhythmia secondary to hypoxia, CCF,
- Pulmonary hypertension
- Increased risk of mortality
- Social and occupational impact
- BMI
- Respiratory exam: usually normal
- Cardio
- BP and fundoscopy: signs of hypertension
- Signs of pulmonary hypertension
- Head and neck: signs of uvular enlargement and macroglossia or tonsillar hypertrophy or orpopharyngeal crowding
- Neck circumference >43cm
- Mallampati classification: seated patient with head in neutral position with mouth wide open and protruded tongue. No phonation, no tongue depressor
- Are they mouth breathers? obligate mouth breathers lose their surfactant
- Polysomnography - Sleep study
- Apnoeas >10secs with at least 5 episodes/hour recorded
- AHI (apnoea hypopnoea index) = total # of apnoeas per night ÷ # hrs slept
- AHI >5 is abnormal but not diagnostic in the absence of symptoms
- Maintenance of Wakefulness Test (MWT)
- TFTs: to exclude hypothyroidism
- Echo: estimation of pulmonary artery pressures, assess right ventricular function
- Non-pharmacological:
- Weight loss
- Avoid/withdraw respiratory depressants
- Avoid EtOH and smoking
- Treat nasal obstruction - vicks vapour etc
- See if patient can buy larger bed, as sound dissipates exponentially
- Devices
- CPAP is gold standard therapy. One of the best rates of adherence. CPAP adherence is > 70%
- Mandible advancement splint
- Surgial correction of upper airways narrowing caused by polyps, enlarged tonsils or macroglossia ; excision of soft tissue in oropharynx
- BiPAP for central sleep apnoea, BUT not adaptive servo-ventilation (increased mortality in large trial)
Obesity Hypoventilation Syndrome
- Clinical syndrome defined by extreme obesity and alveolar hypoventilation during wakefulness
- Prolonged hypoxia and hypercapnia reset the central chemoreceptors
- Characterised by:
- Obesity (BMI >30)
- Somnolence
- Cor pulmonale (pulmonary hypertension)
- Hypercapnic respiratory failure (PCO2 >45)
- Pulmonary function tests: Classically low ERV with restrictive volumes
- High risk of decompensated hypercapnic respiratory failure with intercurrent illness
- Sustained periods of hypoxia and hypercapnia on sleep study
- Often requires BiPAP to blow off their CO2 in hypercapnic respiratory failure
Restless Leg Syndrome
- 5-10% in community based studies
- Can cause insomnia: delayed sleep onset and difficulties maintaining sleep reported by 85%
- Women > males
- 50-60 years
- Higher rates of depression and anxiety in RLS subjects
- Affected QOL (similar to CVA, Parkinson’s)
- 20-25% RLS will be severe/very severe
- Diagnosis
- URGE (1) Urge to move limbs (2) Rest precipitates symptoms (3) Getting up improves symptoms (4) Evening worsens symptoms
- Sleep study not required but will show periodic leg kicks
- Can be primary or secondary (1) Fe deficiency (2) ESKD (3) Pregnancy, especially third trimester (4) drug induced eg TCA (5) Diabetes
- Mx
- Aim to treat secondary causes
- Mainstay of treatment is non pharmacological – only treat pharmacologically if very severe.
- mental alerting activities
- sleep hygeine - abstinence from alcohol, caffeine, nicotine
- evaluate medications that may cause RLS (TCAs, lithium, neuroleptics)
- Pharmacological options:
- Fe replacement if ferritin < 50
- Dopamine agonists are first line – successful in 80% of patients. In 20% of patients they can cause augmentation – paradoxical worsening of symptoms (earlier in the day, spreading).
- α2δ ligands, such as pregabalin, are equally effective, however there is no risk of augmentation. There is a small increase in the risk of suicidal ideation with pregabalin.
- Rescue treatment is with either opioids or long acting benzodiazepines.
Differential diagnosis for daytime somnolence
- Obstructive sleep apnoea
- Narcolepsy
- Obesity hypoventilation syndrome
- Idiopathic hypersomnolence
Idiopathic Hypersomnolence
- excessive daytime somnolence (EDS) even after sufficient or even increased amounts of nightime sleep and without cause
- Clinical features:
- Generally severe and constant EDS
- Longer naps (unrefreshing)
- Protracted daytime drowsiness
- Difficulty awakening from sleep
- Demographics:
- 1-10% EDS sleep clinics
- Maybe heralded by viral illness
- Adolescent (early adulthood)
- A recent study shows that people with IH may have something in their CSF that activates GABA receptors – so it’s like being on Benzo’s all the time
Narcolepsy
- Narcolepsy is a chronic disorder involving the loss of the brain's ability to regulate sleep-wake cycles normally.
- Those with narcolepsy generally experience the REM stage of sleep within 5 minutes of falling asleep, while people who don't have narcolepsy (unless they are significantly sleep deprived) do not experience REM until after a period of slow-wave sleep, which lasts for about the first hour a sleep cycle.
- Risk factors:
- Prevalence 0.05% with cataplexy
- Usually sporadic (familial risk 1-2%)
- Adolescent onset
- HLA association exists
- Associated with obesity
- History and Diagnosis
- Tetrad (10-20%) = Excessive daytime sleepiness, cataplexy (which is diagnostic of narcolepsy alone), sleep paralysis, sleep hallucinations
- Cataplexy - sudden drop of muscle tone triggered by emotion especially laughter or anger. Here you suddenly go into REM sleep
- Hypnagogic [on going to sleep] or hypnopompic hallucinations [on waking up from sleep] (8-70%): auditory, visual or somesthetic
- Sleep Paralysis (5-65%) = inability of move despite being awake (mainly from REM sleep)
- History of cataplexy alone can confirm the diagnosis (70-80%)
- Sleep study (PSG)
- Short REM latency (50%)
- The multiple sleep latency test is used to measure the time elapsed from the start of a daytime nap period to the first signs of sleep, called sleep latency. The test consists of four or five 20-minute nap opportunities set two hours apart, often following an overnight sleep study.
- Narcolepsy can be diagnosed if the mean sleep latency is < 8 minutes (90%) and there are 2+ SOREMPs (which are sleep-onset rapid eye movement periods)
- False positive MSLT can occur if there is: sleep restriction, OSA, drug withdrawal, medications.
- HLA typing is not diagnostic but HLA DR2 (DR15) and DQ1 (DQ6) are associated with narcolepsy
- Hypocretin measurement is being explored further for a diagnostic role: CSF hypocretin < 110 pg/ml is associated with narcolepsy, however <1/3 are normal
- Management
- Non-pharmacological
- Avoidance sleep deprivation
- Proper sleep hygiene
- Maintained of regular sleep-wake schedules (avoid shift work)
- Avoidance of prolonged inactivity during daytime
- Regular scheduled daytime naps (-15 minutes)
- Appropriately times physical activity and caffeinated beverages
- Optimal weight (prone to obesity)
- Avoidance stress
- Regular follow up
- Pharmacological
- Amphetamines such as dexamphetamine, methylphenidate - very effective in daytime somnolence
- Modafanil: first line therapy, wakefulness promoter.
- Cataplexy: SSRIs, TCA (Clomipramine 10-25mg)
- Sodium oxybate TGA approved
- Non-pharmacological
COPD
History
- Symptoms
- Cough, sputum, dyspnoea, wheeze
- Infx Vs Non-Infx exacerbation: fever, coryzal symptoms etc.
- Exercise Tolerance - Usual and current distance
- Exacerbations - frequency, organisms involved (Strep, HIB and Moraxella = most common)
- Smoking history, occupational exposure to dust, coal, fumes, gases
- Vaccination Hx
- Medication Hx and compliance
- FHx of alpha-1 antitrypsin - although alpha-1 antitrypsin deficiency of itself does not improve with enzyme replacement
- Respiratory features of COPD
- Pursed lip breathing
- Cyanosis and nicotine staining
- Prolonged forced exp time > 3sec
- Tracheal tug
- Chest hyperexpansion with evidence of barrel chest
- Decreased BS, wheeze and coarse inspiratory crackles
- Sputum
- Signs of RHF (from cor pulmonale)
- Signs of medication complications
- Spirometry = obstructive, Irreversible obstruction. FEV1/FVC <70%.
- Stage according to COPD-X guidelines (1) Mild: FEV1 60-80% pred (2) Moderate: 40-59% pred (3) Severe: <40% pred
- FEV1 correlates with mortality but does not necessarily correlate with symptoms
- PFT: increased TLC, decreased DLCO
- Sputum culture
- Hb: polycythemia
- WCC, CRP for evidence of infective exacerbation
- ABG: T1RF or T2RF. CO2 retainer? Acidotic = needs BiPAP
- CXR: hyper-inflated
- Normally, diaphragm sits at level of 10th rib posteriorly or 6th rib anterior
- Prominent pulm artery
- Flattened hemi-diaphragm
- Malignancy
- Alpha-1 antitrypsin measurement
- Nutritional assessment: BMI, grip strength, serum alb
- Goals are to Confirm Diagnosis, Optimise Symptoms, Prevent Deterioration, Manage Exacerbations
- Confirm Diagnosis
- Obstructive spirometry with minimal reversibility following bronchodilator
- Remember that overlap syndromes may occur - COPD-Asthma overlap
- Symptoms: Dyspnoea – often multi-factorial [hyperinflation, V/Q mismatching loss of surface area] Cough, Chest tightness and wheeze
- Optimise Symptoms and General non-pharmacological measures
- All patients should have pulmonary rehabilitation: Reduce dyspnoea, improve QOL and reduce hospital admissions, Reduce anxiety, depression and fatigue
- It is an exercise and education program. If in that area such a program does not exist then physiotherapist may be able to do home based exercise
- Education
- Self managed action plan
- Breathlessness increases --> increase bronchodilator
- Breathlessness increases and interferes with ADLs --> short course of corticosteroids
- Increased sputum production --> PO ABx
- Compliance/ inhaler technique
- pharmacists can do a home medicines review
- Self managed action plan
- Nutrition: COPD patients are often cachectic, and this is related to increased mortality
- Chest physiotherapy
- Monitoring for steroid related complications
- Appropriate follow-up
- Support groups
- Pharmacotherapy: Note that whilst most therapies are important in improving symptoms, improving QOL scores and reducing exacerbations
- Short acting bronchodilators
- short acting anticholinergics
- Vaccinations
- Influenza vaccine yearly - mortality reduction
- 23 valent pneumococcal vaccine
- All patients should have pulmonary rehabilitation: Reduce dyspnoea, improve QOL and reduce hospital admissions, Reduce anxiety, depression and fatigue
- Prevent deteriorations
- Addition of long acting bronchodilator if symptoms persist. Check after 6 weeks for improvement in dyspnoea
- LAMA – tiotropium (glycopyrronium, aclidinium)
- LABA: salmeterol, eformoterol
- VLABA: Indacterol (once daily administration)
- Reduced dyspnoea, improved QOL, reduced exacerbations
- If persistent dyspnoea then combination LABA + LAMA
- Use fixed dose inhalers to improve adherence to drug therapy
- FLAME trial - Indacaterol–glycopyrronium was more effective than salmeterol–fluticasone in preventing COPD exacerbations in patients with a history of exacerbation during the previous year N Engl J Med 2016; 374:2222-2234
- If FEV1 <50% and >2 exacerbations per year add Inhaled corticosteroids
- Reduce symptoms, improve quality of life and reduce exacerbations
- But adverse effects are real: pneumonia, easy bruising, cataracts, OP
- If FEV1 < 40% and patient still symptomatic, consider adding low dose theophyline (100mg BD)
- Modest bronchodilator effects
- New data suggesting low dose may have anti-inflammatory and immunomodulatory effects
- Consider long term home oxygen therapy when:
- pO2 < 59mmHg with pulmonary hypertension/RHF
- pO2 < 55mmHg
- Mortality benefit only with ≥ 16 hours/day
- Portable oxygen not shown to have mortality benefit
- Azithromycin
- Shown to reduce exacerbations (Albert et al, NEJM 2011)
- Indicated for use in severe COPD with freq exacerbations
- Does not alter OS
- SEs: Hearing problems, pro-arrythmogenic, Increased colonisation with macrolide resistant organisms
- Addition of long acting bronchodilator if symptoms persist. Check after 6 weeks for improvement in dyspnoea
- Exacerbations
- Greatest predictor is previous exacerbations
- Short acting bronchodilators 4 - 8 puffs SABA q4hrly
- Corticosteroids 30 - 50mg for 5 days then stop, no need to taper
- If infective symptoms then Rx (1) amoxicillin 500mg TDS or doxycycline 200mg first day then 100mg thereafter or (2) if pneumonia treat as such
- Sputum purulence and raised CRP are probably the most useful indicators for need for antibiotics
- Oxygen: used controlled oxygen devices, aim to titrate SpO2 88 - 92%
- NIV: If acidotic and type 2 respiratory failure
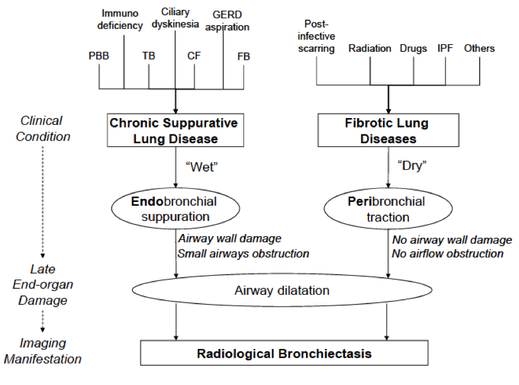
Bronchiectasis
History
- Productive Cough - sputum volume, haemoptysis
- SOB
- Quantify exertional dyspnoea
- Age of diagnosis and what the precipitating condition is
- Colonisers: Long term antibiotics? Frequency of IV
- Associations
- GORD, postnasal drip, sinuses,
- Nutrition, GI, steatorrhoea, weight
- Diabetes, Fertility, Liver function, GORD
- Risk factors/ aetiology :
- Post suppurative lung infection
- Idiopathic
- Cystic fibrosis
- Cilliopathies (Kartagener’s syndrome with situs invertus)
- Congenital hypogammaglobulinaemia
- Childhood infections esp measles and pertussis
- foreign body, luminal mass such as endobronchial or extraluminal malignancy
- ABPA
- Conective tissue disease: RA, Sjogrens with traction bronchiectasis
- Sputum: colour, purulence
- General: barrel chest, increased WOB, BMI, O2,
- Hands: nicotine, clubbing, HPOA
- Chest --> Coarse pan or late inspiratory creps
- CVS: loud P2, RV heave, cor pulmonale
- Situs inversus? à Kartageners (primary ciliary dyskinesis)
- Spirometry – obstructive +/- restrictive
- Bloods & ABG - WCC, CRP, Hb for polycythemia
- Sputum culture: Moraxella, haemophilus, pseudomonas, Staph aureus, Burkholdheria (really poor prognosis)
- CXR: Cystic lesions with Streaky infiltration, Thickened bronchial walls (tram tracking), Dilated airways
- HRCT: bronchiole dilatation with signet sign
- Bronchoscopy: washings for AFB. Remember lady windermere syndrome
- TTE for evidence of cor pulmonale
- CF sweat test looking for elevated [chloride] + genetics
- Serum immunoglobulin levels: IgG/ IgM/ IgA
- Ciliary tests (biopsy or sperm)
- Ix for Aspergillus causing ABPA
- Skin prick test for sensitivity to Aspergillus
- Aspergillus specific IgE
- Raised IgE and FBC eosinophilia
- Sputum Clearance
- PT, Postural drainage, PEP: Flutter valves, mucolytics, hypertonic saline nebs
- Prophylactic Antibiotics should be used only after consultation with a specialist
- Macrolides (azithromycin) if no MAC
- Vaccinations – influenza and pneumococcus
- Monitor Sputum
- Bronchodilators +/- ICS: suppress inflammatory response
- Treat underlying cause
- IVIG for Hypogammaglobulinaemia
- Steroids and azoles (itraconazole) for ABPA
- IVIG for Hypogammaglobulinaemia
- Acute exacerbations (increased sputum volume/ fever/ purulent sputum/ dyspnoea)
- NO Pseudomonas --> amoxycillin
- KNOWN Pseudomonas --> ciprofloxacin
- Haemorrhage
- Minor haemorrhage --> Rx with ABx
- Massive haemorrhage (>250ml) --> CT angiogram with bronchial artery embolisation, bronchoscopy, may need lung resection
- Lung resection of localised disease
Cystic Fibrosis
General BMJ 2016;352:i859
- Multi-system disease with significant respiratory manifestations
- 2000 genetic abnormalities that cause the syndrome of cystic fibrosis
- Autosomal recessive: 1/25 in Caucasian population carry the gene, Incidence 1/2500 in Caucasian population
- CFTR protein
- ATP binding cassette (ABC) family of transporter proteins. ATP hydrolysis is used to drive the opening of the channel
- CFTR protein is to transport anions (such as chloride and bicarbonate) through the apical membrane of epithelial cells, thereby creating an osmotic gradient for fluid secretion. Exception is exocrine sweat glands, where it acts in absorption
- can get lumicaftor and ivakaftor
- G551D stop mutation accounts for 4-5% of CF
- Orally active inhibitor ivakaftor - which is a CFTR potentiator - doubles apical Cl transport
- G551D is a class III gating mutation. Patients have normal amounts of surface CFTR but have problems with gating
- CFTR correctors repair defective CFTR processing by facilitating proper maturation and delivery of protein to the plasma membrane
- These occur in Class II mutations
- Interact directly with CFTR to facilitate its correct folding or by modulating components of the cellular quality control machinery
- Lumacaftor improved CFTR maturation eightfold and enhanced F508del-CFTR mediated chloride transport fourfold
- These occur in Class II mutations
- ATP binding cassette (ABC) family of transporter proteins. ATP hydrolysis is used to drive the opening of the channel
- Diagnosis:
- Neonatal screening tests: Immunereactive tryptase is elevated in carriers and sufferers of CF, If positive -> sweat test (elevated on 2 occasions) and genotype for common CFTR mutations
- [ Need typical phenotypic criterion (sinopulmonary disease OR GI manifestations OR salt loss OR obstructive azospermia) OR positive newborn screening ] AND [(CF in a sibling AND Elevated sweat chloride on at least 2 occasions) OR (Genotype consistent with CF e.g. deltaF508/ deltaF508) OR (Abnormalities in ion transport across airway/nasal epithelium)]
- Multisystem manifestations
- Respiratory: recurrent sinopulmonary disease, airway colonisation, airway obstruction with reactivity, cyst and abscess formation, haemoptysis
- bronchiectasis
- ABPA: classically in upper lobes, right > left in CF sufferers
- pneumothorax
- nasal polyps
- In patients with FEV1 < 30%, almost 100% mortality at 5 years
- Gastrointestinal:
- Meconium ileus in neonates.
- In adults have distal intestinal obstruction syndrome. Almost always occurs in hot weather as they are dehydrated and bowel mucus becomes thick
- GORD: affects 100% CF patients, Number of reasons, principally failure to neutralise gut secretions by pancreas
- Hepatobilliary
- CFTR in the biliary epithelium, not in the hepatocyte. Controls water and solute movement thus promoting bile flow. When CFTR is dysfunctional, it causes thick and tenacious bile that congests intrahepatic bile ducts
- Biliary cirrhosis secondary to bile duct obstruction which can lead to portal hypertension
- 10% incidence of cirrhosis in patients with CF
- Fat soluble vitamin deficiency
- Pancreatic disease
- Exocrine pancreas
- 85% of patients
- Vitamin deficiency
- patients with CF have decreased secretin-stimulated flow through their pancreatic ducts, with mucus so tenacious that decreases secretion of pancreatic enzymes - pancreatic malabsorption
- pancreatitis
- Exocrine pancreas
- Endocrine pancreas
- autolysis secondary to retained enzymes causes CF related diabetes
- CFRD is associated with clinically important declines in pulmonary function and nutritional status, and with increased mortality. Screen with OGTT. HbA1c unreliable in this setting
- Musculoskeletal
- Sero-negative arthropathy
- P-ANCA often positive
- Crush fractures (osteoporosis)
- Genitourinary
- Absent vas deferens
- Male infertility
- Female infertility – not commonly seen.
- Amenorrhoea/anovulatory cycles (relatively common)
- Psychosocial
- Many to talk about
- insight, adherence etc
- Weight, height, muscle bulk, wasting, cachexia, stunted growth
- Venous access: PICC?
- Clubbing, HPOA, tracheal tug
- Evidence bronchiectasis, sputum, creps ULs, ↑FET
- Pulm HTN, Cor Pulmonale, RHF
- Liver transplantation
- Jaundice
- Note there are heaps of management issues to discuss in cystic fibrosis
- Effect of direct dispending vs. self dispensing
- No decline in lung function in those who were given their medication in the clinic compared to the others.
- Average of 11 medications in CF patients
- Adherence to treatment plans is important for good outcomes
- Respiratory: Essentially rests around bronchial toilet and decreasing microbial
- Daily chest Physiotherapy, flutter valves, PEP valves
- 3 monthly sputum cultures
- Mucolytic agents
- Hypertonic saline
- Pulmozyme - this is DNAse
- Decrease airway obstruction and reactivity
- salbutamol, atrovent
- Decrease in microbial content in sputum
- maintenance azithromycin 250mg daily for antimicrobial and inflammatory effect
- If MSSA, flucloxacilin 750mg QID for one month
- If Pseudomonas: neb colistin, neb tobramycin one month alternating
- Mycobacterium absessus --> associated with worse outcome, often multi resistant, large number of centres it is considered a contraindication to lung transplant.
- Burkoldheria cerpacia --> bad bad bad. Effectively 100% mortality
- Will need 2x IVABs if Pseudomonas exacerbation
- Lung transplant
- ↑survivial, ↑QOL, discuss v list (2yr mort >50%)
- If FEV <30% or PaCO2 >50 and O2<55
- Genetics:
- Ivakaftor for the G551D mutations
- Improves FEV1 by 10%
- Lumikaftor + Ivakaftor for delta F508
- Sinus
- Intranasal steroid/NS washout/formal washout
- Exocrine pancreatic insufficiency
- Dietician involvement
- High calorie diet
- Creon for pancreatic enzyme supplementation
- Vitamin supplementation
- Nocturnal NG feeds
- PEG feeding
- CF related diabetes
- insulin therapy if diagnosed
- Psychosocial supports
- CF support groups
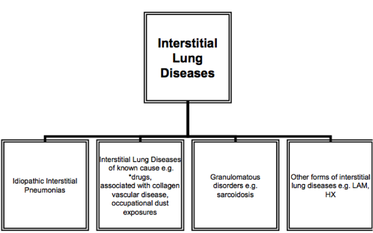
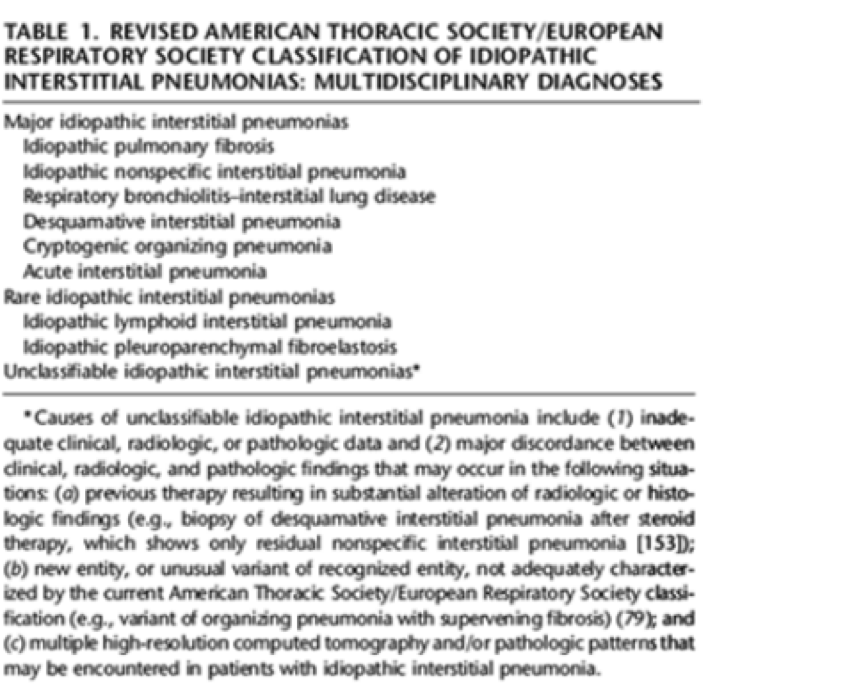
Interstitial Lung Disease
History
- Exertional dyspnoea
- Dry cough
- Lethargy/malaise
- Haemoptysis
- Right heart failure
- Rate of onset of symptoms
- Thorough occupational history
- extrinsic allergies alveolitis (birds, farmers lung), asbestosis, silicosis, beryliosis
- drugs: amiodarone, nitrofunantoin, bleomycin, gold, methotrexate
- ROS for CTD
- rheumatoid arthritis, systemic sclerosis, SLE, polymyositis,dermatomyositis, Sjogren’s, Ank Spon,
- Dry non productive cough
- Cyanosis – peripheral; central if advanced disease
- Clubbing
- Evidence of CTD e.g. RA – symmetrical deforming arthropathy, SS – shiny skin etc
- Radiation tattoos
- Steroid purpura
- Lymphadenopathy in sarcoidosis
- Reduced chest expansion, usually symmetrical
- Fine end-inspiratory crackles
- Upper lobe (SSCHART) - Silicosis, Sarcoidosis, Coal workers pneumoconiosis, Histiocytocis X, Ank Spond, ABPA, Radiation, TB
- Lower lobe (RASIO) - RA, other CTD, Aesbestosis, Scleroderma, IPF, Other (drugs)
- Pulmonary HTN: incr JVP (prominent a wave, systolic v waves), parasternal heave and thrill, RV 3rd or 4th HS, wide split of the 2nd heart sound with loud pulmonary component, peripheral oedema
- Evidence of systemic disease
- Bloods - FBC anaemia or polycythemia; Inflammatory markers ; immunoglobulins ; ANA, ENA, ANCA, CK, RF, SCL-70, myositis panel
- ABG – Type 1 RF
- CXR – bilateral basal reticulonodular infiltrates
- PFT – reduced lung volumes, restrictive, reduced DLCO but preserved KCO until end stage
- Percentage change from baseline FVC (10%) or DLCO (15%) is used traditionally to suggest significant decline
- Percentage change from baseline FVC (10%) or DLCO (15%) is used traditionally to suggest significant decline
- HRCT –The positive predictive value for UIP was over 95% just on HRCT alone, other patterns exist (see respiratory radiology section in short cases)
- MRI – better for upper lobes
- 6MWT – for monitoring, prognosis
- ECHO – pulmonary HTN
- BAL – lymphocytosis, malignant cells, eosinophils
- General supportive measures as discussed in previous respiratory long cases bar the bronchial toilet
- Drugs for IPF
- Pirfenidone
- Reasonably tolerated: GI upset, photosensitivity and LFT disturbance
- Pirfenidone reduced risk of death or disease progression (fall in FVC>10% or 6MWD>50m) by 43%; p=0.0001
- Nintedanib = triple kinase inhibitors
- Block PDGF, VEGF and FGF
- nintedanib reduced the decline in FVC, which is consistent with a slowing of disease progression; nintedanib was frequently associated with diarrhoea, but in IMPULSIS trial this only lead to cessation of drug in 5% of cases
- Pirfenidone
- Non-specific Interstitial Pneumonitis
- Connective tissue related lung fibrosis (most commonly) or may also be idiopathic
- Some response to medical therapy: prednisolone/cyclophosphamide
- Respiratory bronchiolitis-interstitial lung disease
- Lung response to cigarette smoke
- Can be fully reversible if they stop smoking +/- a course of steroids
- Cryptogenic organizing pneumonia
- May be idiopathic or non-specific response
- Infection
- Drug exposure
- 70% improve with steroids
- May be idiopathic or non-specific response
Sarcoidosis
General
- First described in 1989 by dermatologist Caesar Boeck
- defined foci of epithelioid cells with large pale nuclei and giant cells, non caseating granuloma
- Peak incidence 20 - 40
- HLA association
- Two thirds of patients with sarcoidosis generally have a remission within a decade after diagnosis, up to a third of patients have unrelenting disease, leading to clinically significant organ impairment
- Usually asymptomatic, picked up on chest radiography
- Systemic symptoms such as fatigue, night sweats, and weight loss are common; the organ system that is most affected varies with the given patient.
- Löfgren's syndrome, an acute presentation consisting of arthritis, erythema nodosum, and bilateral hilar adenopathy, occurs in 9 to 34% of patients
- 90% of patients, clinical sarcoidosis is manifested as intrathoracic lymph-node enlargement, pulmonary involvement, skin or ocular signs and symptoms, or some combination of these findings.
- Diagnosis of sarcoidosis is reasonably certain without biopsy in patients who present with Löfgren's syndrome.
- In all other cases, a biopsy specimen should be obtained from the involved organ that is most easily accessed, such as the skin, peripheral lymph nodes, lacrimal glands, or conjunctiva
- CNS: The most common problems, listed in decreasing order of frequency, are 1) cranial-nerve palsies, 2) headache, 3) ataxia, 4) cognitive dysfunction, 5) weakness, and 6) seizures.
- Erythema nodosum (raise lesions on L/L) - biopsy shows septal panniculitis
- Maculopapular eruptions
- Lupus Pernio: shiny purple nodules on nose, cheeks, ears, lids
- Uveitis
- Conjunctival nodules (yellow)
- Fundi – papilloedema
- Parotids
- ILD: basal end-inspiratory crackles
- Lymph Nodes
- Abdomen: hepatosplenomegaly
- Joints: non-deforming arthritis
- Neuro: facial nerve palsy
- Cardio Pulse
- Kveim–Siltzbach test has been used for many years in the diagnosis of sarcoidosis. Inject human sarcoid tissue intradermally, look at result in 4 weeks time with biopsy of papule.
- PET may show extent of organ involvement and useful to determine which organ to biopsy
- ACE levels elevated 60% of pts with sarcoid
- CXR radiological staging --> does not correlate to disease severity
- stage 1, bilateral hilar lymphadenopathy without infiltration;
- stage 2, bilateral hilar lymphadenopathy with infiltration;
- stage 3, infiltration alone;
- stage 4, fibrotic bands, bullae, hilar retraction, bronchiectasis, and diaphragmatic tenting.
- 24-hour urinary excretion of calcium should be measured in all patients with sarcoidosis
- Nonprogressive disease does not require treatment
- Progressive disease should be treated with steroids
- Prednisone 1mg/kg for 6 weeks then taper
- Skin lesions can be treated with topical steroids
- Treatments
- Steroids
- NSAIDS
- Cyclosporine
- Cyclophosphamide
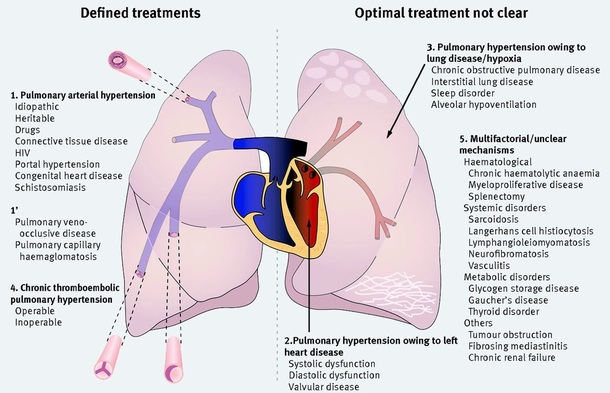
Pulmonary Hypertension
Classification:
- Group 1: Pulmonary arterial hypertension (PAH), which can be idiopathic (IPAH) or associated with other conditions, notably systemic sclerosis and congenital heart disease
- Group 2: Pulmonary hypertension owing to left heart disease (PH-LHD)
- Group 3: Pulmonary hypertension owing to lung disease or hypoxia (PH-Lung), or both
- Group 4: Chronic thromboembolic pulmonary hypertension (CTEPH)
- Group 5: Unclear or multifactorial mechanisms
History
- Exertional dyspnoea
- Fatigue
- Chest pain due to RV dysfunction or left main coronary artery compression by the pulmonary artery
- Syncope - due to RH failure
- RHF – oedema, ascites
- Comment on functional class NYHA
- Assess for potential causes
- FHx
- Previous Ix and Rx
- Possibility of heart lung transplant
- Drugs – Bosentan, sildenafil, inhaled prostacyclin analogue (iloprost)
- Impact on work/ life
- Tachyarrhythmias, most commonly atrial flutter
- Assess severity of dyspnoea – incl on walking
- JVP – large a wave, parasternal impulse, palpable P2, TR
- Early diastolic murmur, pulmonary regurgitation
- Examination findings to suggest underlying cause: CCF, CHD, CTD, signs of DVT, obesity, OSA
- TTE
- Normal RV/RA <25mmHg at rest, <30mmHg exercise
- If RV/RA <30 & DLCO >50% then pHTN unlikely
mPAP 30-40: intermediate likelihood pHTN
mPAP> 40 pHTN likely – further Ix warranted - Test vasoreactivity: usually using inhaled nitric oxide, can identify patients with IPAH who may respond to long term high dose calcium channel blockers. A positive response is defined as a reduction in mean pulmonary artery pressure of at least 10 mm Hg, to less than 40 mm Hg, without a fall in cardiac output
- Right heart cath is always needed to confirm the diagnosis and assess its severity
- Investigations as to aetiology of PH:
- VQ scan to exclude thromboembolic disease
- Spirometry and HRCT chest to Ix ILD/ COPD
- Sleep study --> Ix OSA
- Autoimmune serology
- ANA, dsDNA, ENA, scl70, anti centromere, APL, U1RNP
- HIV serology
- Right and left heart catheterisation
- Other Investigations:
- CXR – prominent pulmonary arteries
- ECG – Right heart strain (R axis deviation, P pulmonale, dominant R wave in V1)
- PFT: Decreased DLCO
- ABG – Type I respiratory failure
- Monitor severity and response with:
- 6 min walk test
- TTE
- Pulmonary hypertension support groups
- Non-pharmacologically optimise heart and lung function
- Treat underlying condition
- Diuretics - ¯ preload, esp RHF + ascites
- Annual flu vaccination is recommended
- Pregnancy should be avoided, it is associated with high mortality, but experience in the management of pulmonary hypertension in pregnancy is increasing. Patients should be transferred to a high risk centre. Mortality 17 - 33%
- Progesterone-only contraceptives—oral desogestrel, intramuscular medroxyprogesterone, and etonogestrel implants—avoid the prothrombotic effects of combined oral contraceptives.
- Recommend termination if pregnancy occurs
- Anticoagulation: warfarin (doubles 3y survival) – indicated for IPAH, hereditary PAH, drug induced (anorexigens) PAH, or group 4 PH
- Oxygen – good for group 3 PH and resting, exercise , or nocturnal hypoxaemia, to qualify need PO2 <60
- Specific pharmacological management
- Drugs are generally indicated for IPH or pHTN secondary to CTD and systemic pulmonary shunts (and only funded for these on PBS) though can be considered on a case by case basis for other forms.
- Long term high dose calcium channel blocker use (diltiazem titrated to 480-720 mg/day or nifedipine titrated to 60-120 mg/day). Use if patient responds to the vasoreactivity test, with 50% showing near normalisation of prognosis!
- Prostanoids: Prostacyclin is a vasodilator with antiproliferative effects
- nebulised iloprost (half life about 30 minutes) improved exercise capacity and haemodynamics when given seven times a day
- Endothelin receptor antagonists:
- bosentan and ambrisentan
- Bosentan causes reversible abnormalities in liver function tests in 5-10% of patients, so monthly monitoring is needed
- PDE5 inhibitors
- Two oral phophodiesterase-5 inhibitors (sildenafil and tadalafil) improved exercise and functional capacity in large well conducted RCTs
- Combination of endothelin and PDE5 inhibitors are used - ambrisentan and tadalafil in combination superior in IPAH than when used individually if WHO class II/ III
- CHEST-1 and CHEST-2: Riociguat significantly improved exercise capacity and pulmonary vascular resistance in patients with chronic thromboembolic pulmonary hypertension N Engl J Med 2013; 369:319-329
- Surgical measures
- Patients with CTEPH may be eligible for pulmonary endarterectomy (2/3)
- Perioperative mortality in large volume centres is now less than 5%.
- Lung transplantation (usually double lung), overall survival 50% at 5y, is indicated in severe PAH or inoperable CTEPH if medical management fails
- atrial septostomy decompresses the pressure loaded heart and may be useful in patients with severe PAH who have intractable syncope but not severe hypoxaemia