Question 1
What is true regarding the toxicity of gentamicin
(A) Gentamicin induced nephrotoxicity increases proportionally with total dose and serum levels
(B) Gentamicin related vestibulotoxicity only occurs at high cumulative doses
(C) Gentamicin related vestibulotoxicity is usually bilateral and symmetrical
(D) Audiometry is the best way to screen for gentamicin induced ototoxicity
(E) Ototoxicity causes a reversible blindness
C: Med J Aust 2012; 196 (11): 701-704
Question 2
What is the most common toxicity associated with PD-1 inhibitors for the treatment of melanoma?
(A) Diarrhoea
(B) Pneumonitis
(C) Fatigue
(D) Rash
(E) Hepatitis
C: N Eng J Med 2015; 372:252-2532
Question 3
What is the risk of methotrexate induced hepatic fibrosis?
(A) 1:100
(B) 1:1000
(C) 1:10000
(D) 1:20000
(E) 1:30000
A: Am J Gastroenterol. 1988;83(12):1337.
Question 4
What is the mechanism of action of aminophyline or theophylline?
(A) Inhibits guanyl cyclase
(B) inhibits Na/K ATPase
(C) Inhibits adenyl cyclase
(D) Inhibits phosphodiesterase
(E) Inhibits P/Q type Ca channels
D: Phosphodiesterase catalyse the conversion of cAMP to AMP, whilst adenyl cyclase catalyses the formation of AMP to cAMP. By inhibiting phosphodiesterase, cAMP concentrations increase thus leading to bronchodilation, cardiac stimulation and vasodilation N Engl J Med 1973; 289:600-603
Question 5
Which of the following medications do not have an active metabolite?
(A) clopidogrel
(B) enalapril
(C) codeine
(D) diazepam
(E) oxycarbazepine
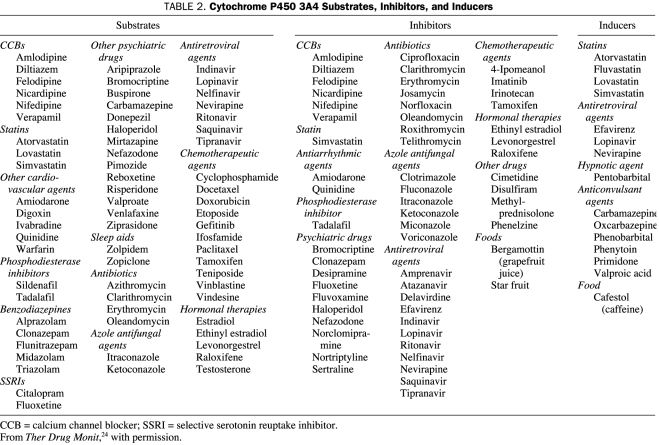
D: enalapril is metabolised to enalaprat, the active agent,. Codeine gets converted to morphine via CYP2D6 Mayo Clin Proc. 2009 Jul; 84(7): 613–624 for table below.
What is true regarding the toxicity of gentamicin
(A) Gentamicin induced nephrotoxicity increases proportionally with total dose and serum levels
(B) Gentamicin related vestibulotoxicity only occurs at high cumulative doses
(C) Gentamicin related vestibulotoxicity is usually bilateral and symmetrical
(D) Audiometry is the best way to screen for gentamicin induced ototoxicity
(E) Ototoxicity causes a reversible blindness
C: Med J Aust 2012; 196 (11): 701-704
Question 2
What is the most common toxicity associated with PD-1 inhibitors for the treatment of melanoma?
(A) Diarrhoea
(B) Pneumonitis
(C) Fatigue
(D) Rash
(E) Hepatitis
C: N Eng J Med 2015; 372:252-2532
Question 3
What is the risk of methotrexate induced hepatic fibrosis?
(A) 1:100
(B) 1:1000
(C) 1:10000
(D) 1:20000
(E) 1:30000
A: Am J Gastroenterol. 1988;83(12):1337.
Question 4
What is the mechanism of action of aminophyline or theophylline?
(A) Inhibits guanyl cyclase
(B) inhibits Na/K ATPase
(C) Inhibits adenyl cyclase
(D) Inhibits phosphodiesterase
(E) Inhibits P/Q type Ca channels
D: Phosphodiesterase catalyse the conversion of cAMP to AMP, whilst adenyl cyclase catalyses the formation of AMP to cAMP. By inhibiting phosphodiesterase, cAMP concentrations increase thus leading to bronchodilation, cardiac stimulation and vasodilation N Engl J Med 1973; 289:600-603
Question 5
Which of the following medications do not have an active metabolite?
(A) clopidogrel
(B) enalapril
(C) codeine
(D) diazepam
(E) oxycarbazepine
D: enalapril is metabolised to enalaprat, the active agent,. Codeine gets converted to morphine via CYP2D6 Mayo Clin Proc. 2009 Jul; 84(7): 613–624 for table below.
Question 6
What is the mechanism by which paracetamol may cause an elevation in INR without an elevation in transaminases?
(A) Paracetamol interferes with the INR assay
(B) Paracetamol interferes directly with enzymes in the vitamin K cycle such as vitamin K dependent gamma carboxylase
(C) NAPQI interferes directly with enzymes in the vitamin K cycle such as vitamin K dependent gamma carboxylase
(D) Paracetamol augments bacterial production of vitamin K
(E) Paracetamol enhances enterohepatic recycling of vitamin K
C: It is NAPQI rather than paracetamol itself that interferes with enzymes involved in the vitamin K cycle, which is where warfarin plays its trick. Thus, there is a real potential for an interaction between warfarin and paracetamol. INR elevation with co-incident transaminitis suggests hepatic dysfunction as the cause of the coagulopathy, rather than interference with the vitamin K cycle. Thromb Haemost. 2004 Oct;92(4):797-802.
Question 7
Which of the following benzodiazepines have the longest half life?
(A) clonazepam
(B) lorazepam
(C) oxazepam
(D) temazepam
(E) diazepam
A: 40 hours!
Question 8
A 45 year old male with generalised epilepsy presents for review at the epilepsy clinic. He is adamant that he is compliant with phenytoin therapy and has attended all clinic appointments so far. He lives with a supportive family and his wife sets reminders every day for him to take his medications. He has recently been seizure free. A phenytoin level was taken and the level was 5 (normal range 10 - 20). He normally takes 100mg/day. What is the best approach to his management?
(A) Refer him to psychology services for advice on optimisation of compliance
(B) Measure peak drug levels
(C) Increase dose to 150mg daily
(D) Increase dose to 200mg daily
(E) Increase dose to 300mg daily
C: If first order kinetics were used, it would be tempting to increase dose by 2 - 3x as the steady state concentration increases with dosing rate according to the following formula C(steady state) = [Bioavailability x dose rate]/[clearance]. Clearance = fraction unbound x intrinsic clearance of drug, which is constant in first order pharmacokinetics. Therefore C(steady state) is proportional to dose rate. In zero-order kinetics, the enzyme is saturated at therapeutic doses. Michaelis menton kinetics for enzymes give v = (Vmax x [S])/(Km + [S]). Applying to pharmacokinetics, with v = C(unbound drug) x Cl (intrinsic), and letting [S] = C(unbound drug), then v = C(unbound drug) x Cl(intrinsic) = (Vmax x Cl(unbound drug))/(Km + C(unbound drug)), which simplifies to Cl(intrinsic) = Vmax/(Km + C(unbound drug)). In first order kinetics, Km >> C(unbound drug) therefore Cl(intrinsic) = Vmax/Km, but in zero-order kinetics where the affinity constant is low (enzymes work potently at low substrate concentrations) then as C(unbound drug increases), Cl(intrinsic) decreases. Therefore dose increments for drugs obeying zero order kinetics must be done cautiously and slowly with repeat monitoring of drug levels thereafter. Aust Prescr 1994;17:36-8
Question 9
Which of the following CYP450 isozymes is involved in the phase 1 metabolism of warfarin?
(A) CYP2E1
(B) CYP3A4
(C) CYP2C9
(D) CYP4A1
(E) CYP2A1
C: BMJ 2015;351:h2391
Question 10
What is FALSE about the use of dabigatran
(A) Of all the directly acting anti-coagulation agents, it is the MOST renally cleared
(B) Dabigatran exilate is the prodrug of dabigatran
(C) Dabigatran has been shown to reduce bleeding rates and stroke in patients with mechanical heart valves
(D) Dabigatran is a direct thrombin inhibitor
(E) If the thrombin time is within the normal value then it effectively rules out the presence of significant dabigatran effect
C: Dabigatran is the only studied DAA in patients with mechanical valves for stroke prophylaxis. The studies showed an increase in stroke rates and an increase in bleeding risk N Engl J Med2013;369:1206-14.
Question 11
Which of the following drugs can be safely administered with dabigatran?
(A) Ketoconazole
(B) Meloxicam
(C) Verapamil
(D) Digoxin
(E) Rifampicin
D: Ketoconazole and verapamil are competitive antagonists of p-glycoprotein efflux pump, as is dabigatran. Meloxicam has a long half life and increases bleeding risk. Rifampicin is a p-glycoprotein inducer and can decrease dabigatran levels. Clin Pharmacokinet. 2008;47(5):285-95.
Question 12
Which of the following drugs exhibit the lowest renal excretion
(A) digoxin
(B) dabigatran
(C) Rivaroxaban
(D) Apixaban
(E) Edoxaban
D: Only 25% of apixaban shows renal excretion. Dabigatran has the greatest renal excretion. BMJ 2015;351:h2391
Question 13 - 16
Select from the following options below, more than one option may be given.
(A) Phase 1
(B) Phase 2
(C) Phase 3
(D) Phase 4
Question 13
Drug X has been shown to have superior efficacy over Drug Y in the management of treatment resistant hypertension in 4 large RCTs. However post-market surveillance reports that Drug X has had increased rates of sarcomas. Consequently a black-box warning is issued for Drug X
D
Question 14
Animal trials have shown effiacy for Drug X in reducing neuronal death in animal models of dementia. Healthy volunteers are exposed to fraction doses and the doses escalated. These patients are monitored very carefuly to determine side-effects and safety profile.
A
Question 15
A large multicentre randomised control trial is underway in determining the efficacy of Drug X over placebo in the treatment of mesothelioma. 2000 patients are enrolled and are divided on a 1:1 randomised basis to drug X versus placebo. The results showed that Drug X significantly decreases progression free survival and overall survival with minimal side effects
C
Question 16
300 patients with hypertension are randomised to receive drug X or placebo.
B
Question 17
Warfarin shows considerable variability in pharmacokinetic response that may be explained by genetic differences. Which is the main genetic polymorphism that effects this variability?
(A) VKORC1
(B) VKORC2
(C) CYP2C9
(D) CYP3A4
(E) CYP 2E1
A: VKORC1 polymoprhisms explain 30% of the dose variation between patients. CYP2C9 explains 10%
What is the mechanism by which paracetamol may cause an elevation in INR without an elevation in transaminases?
(A) Paracetamol interferes with the INR assay
(B) Paracetamol interferes directly with enzymes in the vitamin K cycle such as vitamin K dependent gamma carboxylase
(C) NAPQI interferes directly with enzymes in the vitamin K cycle such as vitamin K dependent gamma carboxylase
(D) Paracetamol augments bacterial production of vitamin K
(E) Paracetamol enhances enterohepatic recycling of vitamin K
C: It is NAPQI rather than paracetamol itself that interferes with enzymes involved in the vitamin K cycle, which is where warfarin plays its trick. Thus, there is a real potential for an interaction between warfarin and paracetamol. INR elevation with co-incident transaminitis suggests hepatic dysfunction as the cause of the coagulopathy, rather than interference with the vitamin K cycle. Thromb Haemost. 2004 Oct;92(4):797-802.
Question 7
Which of the following benzodiazepines have the longest half life?
(A) clonazepam
(B) lorazepam
(C) oxazepam
(D) temazepam
(E) diazepam
A: 40 hours!
Question 8
A 45 year old male with generalised epilepsy presents for review at the epilepsy clinic. He is adamant that he is compliant with phenytoin therapy and has attended all clinic appointments so far. He lives with a supportive family and his wife sets reminders every day for him to take his medications. He has recently been seizure free. A phenytoin level was taken and the level was 5 (normal range 10 - 20). He normally takes 100mg/day. What is the best approach to his management?
(A) Refer him to psychology services for advice on optimisation of compliance
(B) Measure peak drug levels
(C) Increase dose to 150mg daily
(D) Increase dose to 200mg daily
(E) Increase dose to 300mg daily
C: If first order kinetics were used, it would be tempting to increase dose by 2 - 3x as the steady state concentration increases with dosing rate according to the following formula C(steady state) = [Bioavailability x dose rate]/[clearance]. Clearance = fraction unbound x intrinsic clearance of drug, which is constant in first order pharmacokinetics. Therefore C(steady state) is proportional to dose rate. In zero-order kinetics, the enzyme is saturated at therapeutic doses. Michaelis menton kinetics for enzymes give v = (Vmax x [S])/(Km + [S]). Applying to pharmacokinetics, with v = C(unbound drug) x Cl (intrinsic), and letting [S] = C(unbound drug), then v = C(unbound drug) x Cl(intrinsic) = (Vmax x Cl(unbound drug))/(Km + C(unbound drug)), which simplifies to Cl(intrinsic) = Vmax/(Km + C(unbound drug)). In first order kinetics, Km >> C(unbound drug) therefore Cl(intrinsic) = Vmax/Km, but in zero-order kinetics where the affinity constant is low (enzymes work potently at low substrate concentrations) then as C(unbound drug increases), Cl(intrinsic) decreases. Therefore dose increments for drugs obeying zero order kinetics must be done cautiously and slowly with repeat monitoring of drug levels thereafter. Aust Prescr 1994;17:36-8
Question 9
Which of the following CYP450 isozymes is involved in the phase 1 metabolism of warfarin?
(A) CYP2E1
(B) CYP3A4
(C) CYP2C9
(D) CYP4A1
(E) CYP2A1
C: BMJ 2015;351:h2391
Question 10
What is FALSE about the use of dabigatran
(A) Of all the directly acting anti-coagulation agents, it is the MOST renally cleared
(B) Dabigatran exilate is the prodrug of dabigatran
(C) Dabigatran has been shown to reduce bleeding rates and stroke in patients with mechanical heart valves
(D) Dabigatran is a direct thrombin inhibitor
(E) If the thrombin time is within the normal value then it effectively rules out the presence of significant dabigatran effect
C: Dabigatran is the only studied DAA in patients with mechanical valves for stroke prophylaxis. The studies showed an increase in stroke rates and an increase in bleeding risk N Engl J Med2013;369:1206-14.
Question 11
Which of the following drugs can be safely administered with dabigatran?
(A) Ketoconazole
(B) Meloxicam
(C) Verapamil
(D) Digoxin
(E) Rifampicin
D: Ketoconazole and verapamil are competitive antagonists of p-glycoprotein efflux pump, as is dabigatran. Meloxicam has a long half life and increases bleeding risk. Rifampicin is a p-glycoprotein inducer and can decrease dabigatran levels. Clin Pharmacokinet. 2008;47(5):285-95.
Question 12
Which of the following drugs exhibit the lowest renal excretion
(A) digoxin
(B) dabigatran
(C) Rivaroxaban
(D) Apixaban
(E) Edoxaban
D: Only 25% of apixaban shows renal excretion. Dabigatran has the greatest renal excretion. BMJ 2015;351:h2391
Question 13 - 16
Select from the following options below, more than one option may be given.
(A) Phase 1
(B) Phase 2
(C) Phase 3
(D) Phase 4
Question 13
Drug X has been shown to have superior efficacy over Drug Y in the management of treatment resistant hypertension in 4 large RCTs. However post-market surveillance reports that Drug X has had increased rates of sarcomas. Consequently a black-box warning is issued for Drug X
D
Question 14
Animal trials have shown effiacy for Drug X in reducing neuronal death in animal models of dementia. Healthy volunteers are exposed to fraction doses and the doses escalated. These patients are monitored very carefuly to determine side-effects and safety profile.
A
Question 15
A large multicentre randomised control trial is underway in determining the efficacy of Drug X over placebo in the treatment of mesothelioma. 2000 patients are enrolled and are divided on a 1:1 randomised basis to drug X versus placebo. The results showed that Drug X significantly decreases progression free survival and overall survival with minimal side effects
C
Question 16
300 patients with hypertension are randomised to receive drug X or placebo.
B
- Phase I clinical trials
- Focus on pharmacology e.g. mode of delivery, dose finding, dosing schedule
- + safety
- Usually health subjects; n = 15-30
- Volunteers with severe illness may be used, particularly in Oncology trials
- Approximately 70% proceed to phase II
- Phase II clinical trials
- Focus on safety
- + pharmacology and efficacy
- Careful monitoring and continuous assessment
- Usually subjects with target disease; n < 100
- Approximately 50% proceed to phase III
- Phase III clinical trials
- Focus on efficacy
- + Safety and pharmacology
- Subjects with target disease: n = 100-1000s
- Often multi-national, multi-centre
- Approximately 90% proceed to approval
- Phase IV studies
- Focus on long term safety
- Post-marketing surveillance
- Long term follow-up of drug users e.g. use of registries
Question 17
Warfarin shows considerable variability in pharmacokinetic response that may be explained by genetic differences. Which is the main genetic polymorphism that effects this variability?
(A) VKORC1
(B) VKORC2
(C) CYP2C9
(D) CYP3A4
(E) CYP 2E1
A: VKORC1 polymoprhisms explain 30% of the dose variation between patients. CYP2C9 explains 10%