Question 1
Insomnia is the most common sleeping disorder, affecting 10 - 15% of patients worldwide. What is the most common reported symptom?
(A) early morning headache
(B) Trouble initiating sleep
(C) Trouble staying asleep
(D) Early morning Awakening
(E) Restless leg syndrome
C: Trouble maintaining sleep is the most common symptom recognised (61%), followed by early morning awakenings and subsequently difficulty initiating sleep. More than 50% of patients with insomnia disorder will be affected by two out of the three mentioned symptoms. The most common medical association are mood disorders, followed by anxiety disorders. N Engl J Med 2015; 373:1437-1444
Question 2
Which of the following drugs have NOT been used in the treatment of insomnia disorder
(A) Diazepam
(B) Amitryptilline
(C) Fluoxetine
(D) Melatonin
(E) Phenobarbitol
E: Hypnotic agents may be used acutely or chronically in severe refractory insomnia. N Engl J Med 2015; 373:1437-1444
Insomnia is the most common sleeping disorder, affecting 10 - 15% of patients worldwide. What is the most common reported symptom?
(A) early morning headache
(B) Trouble initiating sleep
(C) Trouble staying asleep
(D) Early morning Awakening
(E) Restless leg syndrome
C: Trouble maintaining sleep is the most common symptom recognised (61%), followed by early morning awakenings and subsequently difficulty initiating sleep. More than 50% of patients with insomnia disorder will be affected by two out of the three mentioned symptoms. The most common medical association are mood disorders, followed by anxiety disorders. N Engl J Med 2015; 373:1437-1444
Question 2
Which of the following drugs have NOT been used in the treatment of insomnia disorder
(A) Diazepam
(B) Amitryptilline
(C) Fluoxetine
(D) Melatonin
(E) Phenobarbitol
E: Hypnotic agents may be used acutely or chronically in severe refractory insomnia. N Engl J Med 2015; 373:1437-1444
Question 1
A 68 year old female with chronic intractable dyspnoea secondary to very severe COPD presents to the out-patient department for further management. She is currently optimally managed on medical therapy. You are convinced there is no other reversible cause for her dyspnoea. What is the MOST appropriate management step?
(A) Liase with palliative care
(B) Liase with palliative care and initiate low dose oral morphine
(C) Liase with palliative care and initiate low dose oral benzodiazepines
(D) Enrol her in a clinical trial
(E) Discharge her to palliative care services
B: Internal Medicine Journal 2015; 45(9), 898-904. Low dose morphine has been shown to reduce safely and effectively breathlessness in patients with severe COPD and refractory dyspnoea. However, despite numerous guidelines recommending opioids in this clinical setting, many barriers limit their uptake by clinicians. Integration of palliative care earlier in the disease course can help to improve symptom control for people with severe COPD and refractory breathlessness. A multidisciplinary approach involving both respiratory and palliative care teams offers a new model of care for these patients.
Question 2
At what lung volume is pulmonary vascular resistance lowest?
(A) FRC
(B) RV
(C) [FRV + RV]/ 2
(D) ERV
(E) IRV
A: RPA course 2015
Question 3
What percentage of smokers develop significant disability from COPD?
(A) 5%
(B) 20%
(C) 40%
(D) 60%
(E) 70%
B: RPA lectures 2015
Question 4
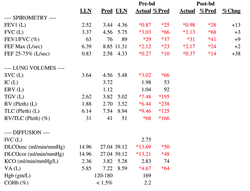
The following is a lung function report from a patient who presented with breathlessness. What is the correct interpretation?
(A) The predominant physiology is obstructive, is COPD-X classification severe with evidence of air-trapping and poor gas mixing
(B) The predominant physiology is mixed, is COPD-X classification severe with evidence of air-trapping and good gas mixing
(C) The predominant physiology is obstructive, is COPD-X classification severe with evidence of reversibility
(D) The predominant physiology is mixed, is COPD-X classification moderate with evidence of reversibility
(E) The predominant physiology is restrictive, there is evidence of air trapping and poor gas mixing
A: Obstructive spirometric ratio as the post bronchodilator ratio is 0.31. As the FEV1 is 28% predicted, this is COPD-X severe (<40% predicted). Air-trapping is indicated based on TLC and RV above 120% predicted. Furthermore gas trapping is likely to be present because Va severely under-estimates TLC.
Question 5
Which of the following is NOT an adverse prognostic marker according to the BODE scale
(A) Body Mass Index <21
(B) Severe obstruction (FEV1 <35% predicted)
(C) Symptomatic dyspnoea on the MRC scale > 4
(D) Significant desaturation on 6MWT
(E) Distance walked in 6MWT
D: Desaturation on 6MWT is not a factor in the BODE index. It is a better predictor than FEV1 of survival. NEJM 2004; 350:1005.
Question 6
What is the function of alpha-1 antitrypsin deficiency in the pathophysiology of emphysema?
(A) It results in increased neutrophil elastase leading to destruction of the lung parenchyma
(B) It results in apical predominant emphysema
(C) It results in sequestered proteins in type II pneumocytes
(D) It results in sequestered proteins in type I pneumocytes
(E) It results in decreased activity of matrix metalloproteinase
A: The emphysema is typicaly panlobular and basal in its distribution. The RAPID trial publised this year showed that alpha 1 antitrypsin augmentation can increase lung density at TLC but not at FRC, paving the way for more randomised clinical trials to assess Alpha 1 anti-trypsin concentrate in patients with severe deficiency (<11). Lancet 2015; 386:360-68.
Question 7
Which of the following lung volumes differentiates the effects of pregnancy from obesity?
(A) FVC
(B) RV
(C) ERV
(D) IC
(E) TLC
B: Residual volume increases in obesity, but decreases in pregnancy. FRC decreases in both pregnancy and obesity. ERV decreases in both, and this is a characteristic of obesity. Clin Chest Med 2011; 32:1 - 13
Question 8
Which of the following factors is the most important physiological change that contributes to decreased aerobic exercise capacity in the elderly?
(A) maximum heart rate
(B) Stroke volume
(C) Gas diffusion
(D) Arterial PaO2
(E) Total lung capacity
A: Maximum heart rate is limited to age by the following equation Max(HR) = 220 - Age. VO2(Max) = CO x O2(extraction = usage). Therefore VO2(Max) = SV.HR.[CaO2 - CvO2], where CaO2 represents arterial oxygen content. SV does decrease in elderly secondary to increased afterload but not to the extent of HR limitation. CaO2 is a product of SaO2 x [Hb] x 1.39. Hb is not significantly altered by ageing, neither is SaO2. In normal subjects HR is the main determinant of maximal exercise capacity because of a lowered HR reserve but in patients with lung disease where ventilator reserve is absent, this is almost always the rate limiting factor. To determine this, the theoretical maximal voluntary ventilation is calculated by the patients FEV1 x 40. Normally the achieved ventilator maximum is 60 - 70% of the theoretical maximal voluntary ventilation (FEV1 x 40). Should measured MVV approach FEV1 x 40, this implies that they do not ventilator reserve. RPA Course 2015
A 68 year old female with chronic intractable dyspnoea secondary to very severe COPD presents to the out-patient department for further management. She is currently optimally managed on medical therapy. You are convinced there is no other reversible cause for her dyspnoea. What is the MOST appropriate management step?
(A) Liase with palliative care
(B) Liase with palliative care and initiate low dose oral morphine
(C) Liase with palliative care and initiate low dose oral benzodiazepines
(D) Enrol her in a clinical trial
(E) Discharge her to palliative care services
B: Internal Medicine Journal 2015; 45(9), 898-904. Low dose morphine has been shown to reduce safely and effectively breathlessness in patients with severe COPD and refractory dyspnoea. However, despite numerous guidelines recommending opioids in this clinical setting, many barriers limit their uptake by clinicians. Integration of palliative care earlier in the disease course can help to improve symptom control for people with severe COPD and refractory breathlessness. A multidisciplinary approach involving both respiratory and palliative care teams offers a new model of care for these patients.
Question 2
At what lung volume is pulmonary vascular resistance lowest?
(A) FRC
(B) RV
(C) [FRV + RV]/ 2
(D) ERV
(E) IRV
A: RPA course 2015
Question 3
What percentage of smokers develop significant disability from COPD?
(A) 5%
(B) 20%
(C) 40%
(D) 60%
(E) 70%
B: RPA lectures 2015
Question 4
The following is a lung function report from a patient who presented with breathlessness. What is the correct interpretation?
(A) The predominant physiology is obstructive, is COPD-X classification severe with evidence of air-trapping and poor gas mixing
(B) The predominant physiology is mixed, is COPD-X classification severe with evidence of air-trapping and good gas mixing
(C) The predominant physiology is obstructive, is COPD-X classification severe with evidence of reversibility
(D) The predominant physiology is mixed, is COPD-X classification moderate with evidence of reversibility
(E) The predominant physiology is restrictive, there is evidence of air trapping and poor gas mixing
A: Obstructive spirometric ratio as the post bronchodilator ratio is 0.31. As the FEV1 is 28% predicted, this is COPD-X severe (<40% predicted). Air-trapping is indicated based on TLC and RV above 120% predicted. Furthermore gas trapping is likely to be present because Va severely under-estimates TLC.
Question 5
Which of the following is NOT an adverse prognostic marker according to the BODE scale
(A) Body Mass Index <21
(B) Severe obstruction (FEV1 <35% predicted)
(C) Symptomatic dyspnoea on the MRC scale > 4
(D) Significant desaturation on 6MWT
(E) Distance walked in 6MWT
D: Desaturation on 6MWT is not a factor in the BODE index. It is a better predictor than FEV1 of survival. NEJM 2004; 350:1005.
Question 6
What is the function of alpha-1 antitrypsin deficiency in the pathophysiology of emphysema?
(A) It results in increased neutrophil elastase leading to destruction of the lung parenchyma
(B) It results in apical predominant emphysema
(C) It results in sequestered proteins in type II pneumocytes
(D) It results in sequestered proteins in type I pneumocytes
(E) It results in decreased activity of matrix metalloproteinase
A: The emphysema is typicaly panlobular and basal in its distribution. The RAPID trial publised this year showed that alpha 1 antitrypsin augmentation can increase lung density at TLC but not at FRC, paving the way for more randomised clinical trials to assess Alpha 1 anti-trypsin concentrate in patients with severe deficiency (<11). Lancet 2015; 386:360-68.
Question 7
Which of the following lung volumes differentiates the effects of pregnancy from obesity?
(A) FVC
(B) RV
(C) ERV
(D) IC
(E) TLC
B: Residual volume increases in obesity, but decreases in pregnancy. FRC decreases in both pregnancy and obesity. ERV decreases in both, and this is a characteristic of obesity. Clin Chest Med 2011; 32:1 - 13
Question 8
Which of the following factors is the most important physiological change that contributes to decreased aerobic exercise capacity in the elderly?
(A) maximum heart rate
(B) Stroke volume
(C) Gas diffusion
(D) Arterial PaO2
(E) Total lung capacity
A: Maximum heart rate is limited to age by the following equation Max(HR) = 220 - Age. VO2(Max) = CO x O2(extraction = usage). Therefore VO2(Max) = SV.HR.[CaO2 - CvO2], where CaO2 represents arterial oxygen content. SV does decrease in elderly secondary to increased afterload but not to the extent of HR limitation. CaO2 is a product of SaO2 x [Hb] x 1.39. Hb is not significantly altered by ageing, neither is SaO2. In normal subjects HR is the main determinant of maximal exercise capacity because of a lowered HR reserve but in patients with lung disease where ventilator reserve is absent, this is almost always the rate limiting factor. To determine this, the theoretical maximal voluntary ventilation is calculated by the patients FEV1 x 40. Normally the achieved ventilator maximum is 60 - 70% of the theoretical maximal voluntary ventilation (FEV1 x 40). Should measured MVV approach FEV1 x 40, this implies that they do not ventilator reserve. RPA Course 2015
Bhatnagar, R. & Maskel, N. The modern diagnosis and management of pleural effusions (2015) BMJ 351
Question 1
A 34 year old male as admitted to the respiratory inpatient unit with progressive shortness of breath. A chest X-ray reveals a large right sided unilateral pleural effusion. An ultrasound guided pleural aspirate is undertaken, the results are shown below:
Pleural fluid pH 7.16
Pleural protein 45 g/dl
Serum protein 50 g/dL
Pleural LDH 342 IU/L
Serum LDH ULN 280 IU/L
Gram stain/ microscopy – no organisms or polymorphs seen
Cytology – atypical cells
What is the most correct response with regards to the pleural fluid analysis
(A) Transudate as the pleural protein is less than the serum protein
(B) Transudate as the serum LDH is less than the pleural LDH
(C) Exudate as the pleural pH < 7.2
(D) Exudate as the pleural protein is > two-thirds the serum protein
(E) Exudate as the pleural LDH : serum LDH is >0.6
E: This is clearly an exudate as it fulfils lights criterion (1: pleural protein: serum protein >0.5, 2: pleural LDH: serum LDH >0.6 or 3: pleural fluid LDH >2/3 ULN of serum LDH). Pleural pH is not a part of lights criterion. A pH <7.2 is strongly indicative of an effusion. Rheumatoid arthritis can also cause this pattern.
Question 2:
A 78 year old patient with metastatic gastric adenocarcinoma is admitted with progressive dyspnoea with super-imposed type 2 respiratory failure. On examination he has stony dullness to both bases, greatest on the right side with bronchial breathing above this area. CT of his chest confirms a large pleural effusion bilaterally. He has both sides drained. The initial analysis shows an exudative effusion and cytology shows atypical cells without any malignant cells seen.
What is the most CORRECT answer
(A) Malignancy is the most common cause of an exudative pleural effusion
(B) Transudative causes are more common than exudative causes of pleural effusion
(C) Talc pleurodesis would be preferred over insertion of an indwelling catheter for the management of his effusion
(D) Pleural fluid cytology has at best a sensitivity of 60%, therefore one cannot rule out malignancy as a cause
(E) Type 2 respiratory failure is not associated with large pleural effusions
D: The sensitivity of cytology is at best 60%. However it is highly specific. Talc pleurodesis obliterates the pleural space in 80% of cases. In the TIME-2 trial, patients with malignant pleural effusions were randomised to receive either standard talc pleurodesis or an indwelling pleural catheter, and the study found no difference between the two arms in the primary end point of patient reported dyspnoea at six weeks. Indwelling catheters can be left in for many months and even years without change, and there is a low risk of infection. Furthermore, if they do get infected then they do not necessarily need to be removed. Talc has been shown to be the best at producing a chemical pleurodesis. Exudates account for 57% of all pleural effusions according to the BMJ review, and ofthese infections are more common than malignancy. Type 2 respiratory failure may occur due to a failure of ventilation, given decreased tdal volume not overcome by increased respiratory rate.
Question 3
A 52 year old female who suffers from chronic alcoholism is seen in emergency after failure to cope. She is hypotensive and tachycardic. Her chest X-ray shows a large left sided pleural effusion that causes midline shift. Initial diagnostic thoracocentecis shows an exudative effusion with gram stain showing gram positive rods. Her pleural pH is 7.16. She is taken to theartre and underwent a thoracotomy and drainage. Unfortunately her inflammatory markers continued to rise and she had persistent low grade temperatures. A repeat Chest X-ray showed re-accumulation of the fluid. A chest drain is re-inserted. In addition to the chest drain, what additional step would you take?
(A) TpA (alteplase) + DNAse alpha into drain
(B) TpA alone
(C) DNAse alpha alone
(D) Urokinase alone
(E) Streptokinase and Urokinase
A: Combination of TpA and DNAse alpha is better than either alone according to the MIST-2 trial published in the new england journal of medicine. It improved fluid drainage in patients with pleural infection and reduced the frequency of surgical referral and the duration of the hospital stay compared to single agent therapy N Engl J Med 2011; 365:518-526
Question 1
A 34 year old male as admitted to the respiratory inpatient unit with progressive shortness of breath. A chest X-ray reveals a large right sided unilateral pleural effusion. An ultrasound guided pleural aspirate is undertaken, the results are shown below:
Pleural fluid pH 7.16
Pleural protein 45 g/dl
Serum protein 50 g/dL
Pleural LDH 342 IU/L
Serum LDH ULN 280 IU/L
Gram stain/ microscopy – no organisms or polymorphs seen
Cytology – atypical cells
What is the most correct response with regards to the pleural fluid analysis
(A) Transudate as the pleural protein is less than the serum protein
(B) Transudate as the serum LDH is less than the pleural LDH
(C) Exudate as the pleural pH < 7.2
(D) Exudate as the pleural protein is > two-thirds the serum protein
(E) Exudate as the pleural LDH : serum LDH is >0.6
E: This is clearly an exudate as it fulfils lights criterion (1: pleural protein: serum protein >0.5, 2: pleural LDH: serum LDH >0.6 or 3: pleural fluid LDH >2/3 ULN of serum LDH). Pleural pH is not a part of lights criterion. A pH <7.2 is strongly indicative of an effusion. Rheumatoid arthritis can also cause this pattern.
Question 2:
A 78 year old patient with metastatic gastric adenocarcinoma is admitted with progressive dyspnoea with super-imposed type 2 respiratory failure. On examination he has stony dullness to both bases, greatest on the right side with bronchial breathing above this area. CT of his chest confirms a large pleural effusion bilaterally. He has both sides drained. The initial analysis shows an exudative effusion and cytology shows atypical cells without any malignant cells seen.
What is the most CORRECT answer
(A) Malignancy is the most common cause of an exudative pleural effusion
(B) Transudative causes are more common than exudative causes of pleural effusion
(C) Talc pleurodesis would be preferred over insertion of an indwelling catheter for the management of his effusion
(D) Pleural fluid cytology has at best a sensitivity of 60%, therefore one cannot rule out malignancy as a cause
(E) Type 2 respiratory failure is not associated with large pleural effusions
D: The sensitivity of cytology is at best 60%. However it is highly specific. Talc pleurodesis obliterates the pleural space in 80% of cases. In the TIME-2 trial, patients with malignant pleural effusions were randomised to receive either standard talc pleurodesis or an indwelling pleural catheter, and the study found no difference between the two arms in the primary end point of patient reported dyspnoea at six weeks. Indwelling catheters can be left in for many months and even years without change, and there is a low risk of infection. Furthermore, if they do get infected then they do not necessarily need to be removed. Talc has been shown to be the best at producing a chemical pleurodesis. Exudates account for 57% of all pleural effusions according to the BMJ review, and ofthese infections are more common than malignancy. Type 2 respiratory failure may occur due to a failure of ventilation, given decreased tdal volume not overcome by increased respiratory rate.
Question 3
A 52 year old female who suffers from chronic alcoholism is seen in emergency after failure to cope. She is hypotensive and tachycardic. Her chest X-ray shows a large left sided pleural effusion that causes midline shift. Initial diagnostic thoracocentecis shows an exudative effusion with gram stain showing gram positive rods. Her pleural pH is 7.16. She is taken to theartre and underwent a thoracotomy and drainage. Unfortunately her inflammatory markers continued to rise and she had persistent low grade temperatures. A repeat Chest X-ray showed re-accumulation of the fluid. A chest drain is re-inserted. In addition to the chest drain, what additional step would you take?
(A) TpA (alteplase) + DNAse alpha into drain
(B) TpA alone
(C) DNAse alpha alone
(D) Urokinase alone
(E) Streptokinase and Urokinase
A: Combination of TpA and DNAse alpha is better than either alone according to the MIST-2 trial published in the new england journal of medicine. It improved fluid drainage in patients with pleural infection and reduced the frequency of surgical referral and the duration of the hospital stay compared to single agent therapy N Engl J Med 2011; 365:518-526

Question 1
A 34 year old female suffering deltaF508/deltaF508 homozygous cystic fibrosis presents to the CF clinic with worsening chest pain, brown sputum production and progressive deterioration in self reported FEV1. Initial bloods reveal an elevated white cell count, total IgE of ~ 1600 and elevated serum eosinophils. Her chest X-ray is shown below
What is the most likely diagnosis?
(A) Allergic Bronchopulmonary Aspergillosis
(B) Right upper lobe bronchopneumonia
(C) Pulmonary embolus
(D) Pneumothorax
(E)mycobacterium abscessus infection
A: Right upper lobe consolidation, increased chest pain, progressive breathlessness, decline in FEV1, eosinophilia with raised IgE are classic of ABPA. ABPA occurs in 15% of CF patients. They should be treated with corticosteroids and either itraconazole or voriconazole. Itraconazole given for 16 weeks appears to be steroid sparing (Thorax 70:270, 2015), decreasing number of exacerbations. IgE >1500 signifies severe disease, however >5000 would imply a diagnosis of atopic dermatitis (RPA lecture series 2015, PEP lectures 2015)
Question 2
What is the median survival of a patient with cystic fibrosis
(A) 25 years
(B) 32 years
(C) 41 years
(D) 55 years
(E) 62 years
C: Data from 2014 indicate that median survival is 41 years. The oldest patient at the RPA clinic is 66 years apparently!
Question 3
Females tend to die quicker of CF and have exacerbations during the follicular phase of their menstrual cycle. What is the rationale for this
(A) Increased progesterone increases the viscosity of the mucous secretions
(B) Increased oestrogen is correlated with increased viscosity of mucous secretions
(C) Increased oestrogen is associated with increased destructive cytopathic inflammation
(D) Increased progesterone decreases the activity of non-pathogenic respiratory flora increasing the relative proportion of pathogenic bacteria such as pseudomonas aeuroginosa
(E) Increased oestrogen directly increases the concentration of mycobacterium abscessus.
B: Accoring to a NEJM publication, Increased oestrogen during the follicular phase increases sputum viscosity, and therefore leads to increased exacerbations during this phase of the menstrual cycle in females N Engl J Med 2015; 372:351-362.
Question 4
How many classes of mutations are there in cystic fibrosis?
(A) 3
(B) 4
(C) 5
(D) 6
(E) 7
C: The first 3 mutations are known to decrease CFTR function and are more severe. Class 1 includes deltaF508, class 3 includes G551D, a mutation class that can benefit from ivakaftor, a channel potentiator. Lumicaftor combined with ivakaftor for deltaF508 has shown some benefit in research trials but is not yet available in Australia on the PBS. Ivakaftor is liscenced through the PBS for CF patients with G551D mutation or other Class 3 gating mutations. It cannot be given with CYP3A4 inducers (PBS.gov.au, RPA lecture 2015 Prof Peter Bye).
Question 5
A 38 year old female with cystic fibrosis develops an acute exacerbation of her cystic fibrosis during the follicular phase of her menstrual cycle. She has a stormy course coinciding with progressive decline in FEV1 and type 2 respiratory failure. Sputum culture isolates show Burkholderia cepacia. With regards to this pathogen, what is FALSE
(A) The 1 year mortality is 40%
(B) Pathogen fails to respond to ahminoglycosides, tazocin and ceftazadine
(C) Chloramphenicol has been used as a treatment in these patients
(D) It is associated with a POOR prognosis
A: The 1 year mortality approaches 62% (Stanford Antimicrobial guidelines 2015). Unfortunately many patients colonised with B. cepacia are not transplant candidates due to a significant one year mortality.
Question 6
What is FALSE regarding the pathology of cystic fibrosis
(A) Oestrogen increases the viscosity of mucus secretions
(B) Thick mucus secretions are due to hyper-absorption of Na in mucus, leading to osmotic dehydration of mucus
(C) Acidic mucus due to defect in bicarbonate secretion through the CFTR channel may account, in part, for decreased intraluminal airway defence
(D) CFTR may play an important role in development of the upper airways during embryogenesis
(E) A combination of impaired mucocilliary transport and impaired antimicrobial defence may account for the fact that cystic fibrosis tends to a poorer prognosis compared to primary colliery dyskinesia.
B: Hyper-absorption of Na through ENaC channels were once thought to be responsible for impaired mucocilliary transport. All the other elements are true. N Engl J Med 2015; 372:351-362
Question 7
A 32 year old male presents to the respiratory clinic with persistent productive cough since a child. He has always been exquisitely prone to develop chest infections. Unfortunately, he is also infertile. Investigations reveal normal immunoglobulins, normal sweat sodium/ chloride, negative skin prick for avian antigens and aspergillus. What is the most likely diagnosis?
(A) Bronchiectesis
(B) Bronchiolitis obliterates
(C) Primary Ciliary Dyskinesia
(D) Kartegeners syndrome
(E) Cystic Fibrosis
C: This is due to a partial or complete deficienty of outer or inner dyne arms of cilia with poor beating. If it is associated with dextrocardia and situs inverts then it is called Kartagener's syndrome. These patients are also infertile. Cystic fibrosis stem would have an elevated sweat sodium and chloride level however care must be taken in interpreting this result in adults. Cystic fibrosis patients have a failure of their vas deferens development. There testes are normal, as is its response to LH and FSH. N Engl J Med 2011; 364:1533-1543
Question 8
A 64 year old female presents to the emergency department with type 1 respiratory failure. She has had a chronic cough, fevers and night sweats. She has recently moved to Adelaide after 10 years living in the Northern Territory. Recently her house was rendered unliveable after 2 weeks of chronic wet season associated rains. She has diabetes, chronic liver disease and COPD. Her chest X-ray shows military infiltrates
Which of the following treatment options would be most appropriate?
(A) Rifampicine, Isoniazid, Pyrazinamide, Ethambutol
(B) Benzylpenicllin and doxycycline
(C) Tazocin
(D) Ceftriaxone and Azithromycin
(E) Meropenem
E: This patient is most likely to have melioidosis, which is caused by the gram negative bacillus burkholderia pseudomallei. This organism is found in the soil and rice paddies of SE Asia and Northern Australia, and should be included in the differential diagnosis of any patient presenting with respiratory distress from these regions. CXR may be similar to miliary TB. Neurological melioidosis, abscesses, cutaneous lesions, septic arthritis and osteomyelitis also occur. Treatment must occur for greater than 14 days with ceftazadime or meropenem. Pulmonary TB is also in the differential diagnosis but the stem was pointing strongly towards melioidosis. Patients with diabetes often have more severe disease. Oral therapy after initial IV therapy consists of bactrim AND doxycycline. Clin Microbiol Rev 18: 383, 2005
Question 9
Which of the following organisms if isolated in patients with cystic fibrosis is associated with a particularly poor outcome?
(A) Burkholderia cepacia
(B) Pseudomonas aeruginosa
(C) MRSA
(D) MSSA
(E) Actinomycetes myeri
A: Patients who have B. cepacia have a very high associated mortality. The cepacia syndrome is associated with a necrotising cavitating pneumonia. Am J Respir Crit Care Med. 2001; 164:2102 - 2106
A 34 year old female suffering deltaF508/deltaF508 homozygous cystic fibrosis presents to the CF clinic with worsening chest pain, brown sputum production and progressive deterioration in self reported FEV1. Initial bloods reveal an elevated white cell count, total IgE of ~ 1600 and elevated serum eosinophils. Her chest X-ray is shown below
What is the most likely diagnosis?
(A) Allergic Bronchopulmonary Aspergillosis
(B) Right upper lobe bronchopneumonia
(C) Pulmonary embolus
(D) Pneumothorax
(E)mycobacterium abscessus infection
A: Right upper lobe consolidation, increased chest pain, progressive breathlessness, decline in FEV1, eosinophilia with raised IgE are classic of ABPA. ABPA occurs in 15% of CF patients. They should be treated with corticosteroids and either itraconazole or voriconazole. Itraconazole given for 16 weeks appears to be steroid sparing (Thorax 70:270, 2015), decreasing number of exacerbations. IgE >1500 signifies severe disease, however >5000 would imply a diagnosis of atopic dermatitis (RPA lecture series 2015, PEP lectures 2015)
Question 2
What is the median survival of a patient with cystic fibrosis
(A) 25 years
(B) 32 years
(C) 41 years
(D) 55 years
(E) 62 years
C: Data from 2014 indicate that median survival is 41 years. The oldest patient at the RPA clinic is 66 years apparently!
Question 3
Females tend to die quicker of CF and have exacerbations during the follicular phase of their menstrual cycle. What is the rationale for this
(A) Increased progesterone increases the viscosity of the mucous secretions
(B) Increased oestrogen is correlated with increased viscosity of mucous secretions
(C) Increased oestrogen is associated with increased destructive cytopathic inflammation
(D) Increased progesterone decreases the activity of non-pathogenic respiratory flora increasing the relative proportion of pathogenic bacteria such as pseudomonas aeuroginosa
(E) Increased oestrogen directly increases the concentration of mycobacterium abscessus.
B: Accoring to a NEJM publication, Increased oestrogen during the follicular phase increases sputum viscosity, and therefore leads to increased exacerbations during this phase of the menstrual cycle in females N Engl J Med 2015; 372:351-362.
Question 4
How many classes of mutations are there in cystic fibrosis?
(A) 3
(B) 4
(C) 5
(D) 6
(E) 7
C: The first 3 mutations are known to decrease CFTR function and are more severe. Class 1 includes deltaF508, class 3 includes G551D, a mutation class that can benefit from ivakaftor, a channel potentiator. Lumicaftor combined with ivakaftor for deltaF508 has shown some benefit in research trials but is not yet available in Australia on the PBS. Ivakaftor is liscenced through the PBS for CF patients with G551D mutation or other Class 3 gating mutations. It cannot be given with CYP3A4 inducers (PBS.gov.au, RPA lecture 2015 Prof Peter Bye).
Question 5
A 38 year old female with cystic fibrosis develops an acute exacerbation of her cystic fibrosis during the follicular phase of her menstrual cycle. She has a stormy course coinciding with progressive decline in FEV1 and type 2 respiratory failure. Sputum culture isolates show Burkholderia cepacia. With regards to this pathogen, what is FALSE
(A) The 1 year mortality is 40%
(B) Pathogen fails to respond to ahminoglycosides, tazocin and ceftazadine
(C) Chloramphenicol has been used as a treatment in these patients
(D) It is associated with a POOR prognosis
A: The 1 year mortality approaches 62% (Stanford Antimicrobial guidelines 2015). Unfortunately many patients colonised with B. cepacia are not transplant candidates due to a significant one year mortality.
Question 6
What is FALSE regarding the pathology of cystic fibrosis
(A) Oestrogen increases the viscosity of mucus secretions
(B) Thick mucus secretions are due to hyper-absorption of Na in mucus, leading to osmotic dehydration of mucus
(C) Acidic mucus due to defect in bicarbonate secretion through the CFTR channel may account, in part, for decreased intraluminal airway defence
(D) CFTR may play an important role in development of the upper airways during embryogenesis
(E) A combination of impaired mucocilliary transport and impaired antimicrobial defence may account for the fact that cystic fibrosis tends to a poorer prognosis compared to primary colliery dyskinesia.
B: Hyper-absorption of Na through ENaC channels were once thought to be responsible for impaired mucocilliary transport. All the other elements are true. N Engl J Med 2015; 372:351-362
Question 7
A 32 year old male presents to the respiratory clinic with persistent productive cough since a child. He has always been exquisitely prone to develop chest infections. Unfortunately, he is also infertile. Investigations reveal normal immunoglobulins, normal sweat sodium/ chloride, negative skin prick for avian antigens and aspergillus. What is the most likely diagnosis?
(A) Bronchiectesis
(B) Bronchiolitis obliterates
(C) Primary Ciliary Dyskinesia
(D) Kartegeners syndrome
(E) Cystic Fibrosis
C: This is due to a partial or complete deficienty of outer or inner dyne arms of cilia with poor beating. If it is associated with dextrocardia and situs inverts then it is called Kartagener's syndrome. These patients are also infertile. Cystic fibrosis stem would have an elevated sweat sodium and chloride level however care must be taken in interpreting this result in adults. Cystic fibrosis patients have a failure of their vas deferens development. There testes are normal, as is its response to LH and FSH. N Engl J Med 2011; 364:1533-1543
Question 8
A 64 year old female presents to the emergency department with type 1 respiratory failure. She has had a chronic cough, fevers and night sweats. She has recently moved to Adelaide after 10 years living in the Northern Territory. Recently her house was rendered unliveable after 2 weeks of chronic wet season associated rains. She has diabetes, chronic liver disease and COPD. Her chest X-ray shows military infiltrates
Which of the following treatment options would be most appropriate?
(A) Rifampicine, Isoniazid, Pyrazinamide, Ethambutol
(B) Benzylpenicllin and doxycycline
(C) Tazocin
(D) Ceftriaxone and Azithromycin
(E) Meropenem
E: This patient is most likely to have melioidosis, which is caused by the gram negative bacillus burkholderia pseudomallei. This organism is found in the soil and rice paddies of SE Asia and Northern Australia, and should be included in the differential diagnosis of any patient presenting with respiratory distress from these regions. CXR may be similar to miliary TB. Neurological melioidosis, abscesses, cutaneous lesions, septic arthritis and osteomyelitis also occur. Treatment must occur for greater than 14 days with ceftazadime or meropenem. Pulmonary TB is also in the differential diagnosis but the stem was pointing strongly towards melioidosis. Patients with diabetes often have more severe disease. Oral therapy after initial IV therapy consists of bactrim AND doxycycline. Clin Microbiol Rev 18: 383, 2005
Question 9
Which of the following organisms if isolated in patients with cystic fibrosis is associated with a particularly poor outcome?
(A) Burkholderia cepacia
(B) Pseudomonas aeruginosa
(C) MRSA
(D) MSSA
(E) Actinomycetes myeri
A: Patients who have B. cepacia have a very high associated mortality. The cepacia syndrome is associated with a necrotising cavitating pneumonia. Am J Respir Crit Care Med. 2001; 164:2102 - 2106
Question 10
Which of the following conditions is associated with a neutrophilic cellular pattern on Bronchio-alveolar lavage?
(A) Idiopathic pulmonary fibrosis
(B) Hypersensitivity pneumonitis
(C) Cryptogenic organising pneumonia
(D) Drug induced pneumonitis
(E) Radiation pneumonitis
A: IPF is the only condition associated with a neutrophilic (>3%) cellular pattern. The other options are associated with a lymphocytic cellular pattern. Am J Resp Crit Med 2012 Vol 185 1006
Question 11
What is the most common cause of clubbing?
(A) respiratory disorders
(B) congenital heart disease
(C) infective endocarditis
(D) idiopathic clubbing
(E) Chronic liver disease
A: In one study, 80% had respiratory disorders, and only 5 - 10% had idiopathic or hereditary clubbing.
Which of the following conditions is associated with a neutrophilic cellular pattern on Bronchio-alveolar lavage?
(A) Idiopathic pulmonary fibrosis
(B) Hypersensitivity pneumonitis
(C) Cryptogenic organising pneumonia
(D) Drug induced pneumonitis
(E) Radiation pneumonitis
A: IPF is the only condition associated with a neutrophilic (>3%) cellular pattern. The other options are associated with a lymphocytic cellular pattern. Am J Resp Crit Med 2012 Vol 185 1006
Question 11
What is the most common cause of clubbing?
(A) respiratory disorders
(B) congenital heart disease
(C) infective endocarditis
(D) idiopathic clubbing
(E) Chronic liver disease
A: In one study, 80% had respiratory disorders, and only 5 - 10% had idiopathic or hereditary clubbing.
Question 1:
A 23 year old male with metastatic germ cell testicular cancer treated with bleomycin/ cisplatin combination presents 6 months after with progressive breathlessness and non-productive cough. Examination reveals hypoxia to 85% RA, tachycardia and decreased air-entry with fine bibasilar end inspiratory crackles. CXR reveals blunting of the costophrenic angles with sub-pleural opacification. Lung function tests reveal a total lung capacity of 65%, normal spirometry and DLCO of 68% predicted, correctable for alveolar volume. A diagnosis of bleomycin induced pulmonary fibrosis is made. Out of the following statements with regards to this patient, what is FALSE.
(A) 60% of bleomycin is cleared by the liver
(B) Risk factors for bleomycin induced pulmonary disease include age, cumulative dose, renal function, cigarette smoke, and other chemotherapy such as cisplatin
(C) Different phenotypes of bleomycin pulmonary toxicity exist, including subacute pulmonary fibrosis, organising pneumonia, acute chest pain syndrome during infusion and hypersensitivity pneumonitis
(D) Anecdotal studies suggest that supplemental oxygen may be deleterious, therefore the guidelines suggest maintaining oxygen saturations between 88 – 92%
(E) bleomycin hydroxylase, whilst abundant in most tissues, is mostly absent from the skin and lung, in part explaining pulmonary toxicity
A: 80% of bleomycin is cleared by the kidneys explaining renal dysfunction as a risk factor for pulmonary toxicity. In patients with hypersensitivity pneumonitis or organising pneumonia, high dose glucocorticoids are recommended in the management of the patient. It is only anecdotal studies that suggest avoiding oxygen therapy in this condition. Bleomycin seems to exert its chemotherapeutic effect and pulmonary toxicity by forming complexes with oxygen, ferric Fe and inducing breaks in dsDNA (uptodate)
Question 2
What is the most common radiological pattern of lung involvement seen in patients with interstitial fibrosis secondary to connective tissue disease?
(A) Usual interstitial pneumonia
(B) Lymphocytic Interstitial Pneumonia
(C) Hypersensitivity pneumonitis pattern
(D) Non-specific Interstitial Pneumonia pattern
(E) Bronchiolitis obliterans organising pneumonia
D: UIP histology suggested by architectural distortion, patchy changes showing spatial and temporal heterogeneity and fibroblastic foci (pathognomonic) – RPA course, PEP lecture 2014
A: Prone HRCT is really only done in patients being investigated for IPF to showcase the early fibrotic changes. The sub-pleural septal and interlobular thickening with subpleural honeycombing is usually basal and posterior, therefore these changes are brought out by gravitational positioning in the prone position. Other radiological changes include sub-pleural honeycombing and traction bronchiectasis. Ground glass changes are seen in NSIP. Granulomas and upper lobe predominance is sarcoidosis, nodules is hypersensitivity pneumonitis (RPA lecture).
Question 4
What is the most important predictor of mortality in patients with idiopathic pulmonary fibrosis?
(A) DLCO
(B) 6MWT distance
(C) FVC drop of 10% in 6 months
(D) Age
(E) Male gender
C: According to PEP 2014 lecture
Question 5
What is the most common lung function test pattern seen in a patient with IPF?
(A) FEV1/ FVC <0.7, TLC >80% predicted, DLCO <80% but correctable for Va
(B) FEV1/ FVC >0.7, TLC <80% predicted, DLCO >80% but correctable for Va
(C) FEV1/ FVC >0.7, TLC >80% predicted, DLCO <80% but not-correctable for Va
(D) FEV1/ FVC >0.7, TLC <80% predicted, DLCO <80% but not-correctable for Va
(E) FEV1/ FVC >0.7, TLC <80% predicted, DLCO <80% but correctable for Va
E: Non-obstructive spirometry, restrictive lung volumes with reduced DLCO corrected for by alveolar volumes (PEP 2014, RPA course Dr Lauren Troy)
Question 6
In the ASCEND and CAPACITY trials looking at pirfenidone, what was the most common reported adverse event of pirfenidone compared to placebo?
(A) Insomnia
(B) Headache
(C) Rash
(D) Nausea
(E) Vomiting
D: Nausea was reported in 100% of patients. Other SE that were more commonly reported compared to placebo include Insomnia, rash and vomiting (1)
Question 7
Pooling the results of Pirfenidone trials in patients with IPF (ASCEND, CAPACITY 1 and CAPACITY 2), which of the following results is FALSE
(A) Decreased deaths (when pooled) related to Idiopathic pulmonary fibrosis
(B) Decreased deaths (when pooled) related to all cause mortality
(C) Reduction in decline of 6MWT
(D) Improvement in dyspnoea scores
(E) Reduction in decline of FVC
D:
Question 8
A 79 year old female from the country is referred to RPAH with pulmonary alveolar proteinosis secondary to JAK2 negative myelofibrosis. Her exercise tolerance has been gradually declining over the last year, however she has noticed a rapid decline in the last 3 weeks. She has reduced FEV1 compared to her baseline, and is coughing up more brown coloured sputum. With regards to her potential diagnosis, what is NOT an appropriate management step
(A) Admission for IV antibiotics for a presumed infective exacerbation of PAP
(B) Discussion with anaesthetics regarding whole lung lavage under ECMO support
(C) Pulse methylprednisolone and cyclophosphamide, with TMPT levels prior to azathioprine maintenance
(D) Intensive physiotherapy, hypertonic saline nebs and oxygen therapy to maintain saturations
(E) Optimising the management of her myelofibrosis
C: High dose immunosuppression has no role in this condition. Rare haematological conditions have been associated with PAP, an overall very rare disease in ILD clinics! Idiopathic PAP may be associated with antibodies to GM-CSF, and trials have generally been unyielding when patients with PAP have been given GM-CSF.
1. King TE, Jr., Bradford WZ, Castro-Bernardini S, Fagan EA, Glaspole I, Glassberg MK, et al. A phase 3 trial of pirfenidone in patients with idiopathic pulmonary fibrosis. N Engl J Med. 2014;370(22):2083-92.
A 23 year old male with metastatic germ cell testicular cancer treated with bleomycin/ cisplatin combination presents 6 months after with progressive breathlessness and non-productive cough. Examination reveals hypoxia to 85% RA, tachycardia and decreased air-entry with fine bibasilar end inspiratory crackles. CXR reveals blunting of the costophrenic angles with sub-pleural opacification. Lung function tests reveal a total lung capacity of 65%, normal spirometry and DLCO of 68% predicted, correctable for alveolar volume. A diagnosis of bleomycin induced pulmonary fibrosis is made. Out of the following statements with regards to this patient, what is FALSE.
(A) 60% of bleomycin is cleared by the liver
(B) Risk factors for bleomycin induced pulmonary disease include age, cumulative dose, renal function, cigarette smoke, and other chemotherapy such as cisplatin
(C) Different phenotypes of bleomycin pulmonary toxicity exist, including subacute pulmonary fibrosis, organising pneumonia, acute chest pain syndrome during infusion and hypersensitivity pneumonitis
(D) Anecdotal studies suggest that supplemental oxygen may be deleterious, therefore the guidelines suggest maintaining oxygen saturations between 88 – 92%
(E) bleomycin hydroxylase, whilst abundant in most tissues, is mostly absent from the skin and lung, in part explaining pulmonary toxicity
A: 80% of bleomycin is cleared by the kidneys explaining renal dysfunction as a risk factor for pulmonary toxicity. In patients with hypersensitivity pneumonitis or organising pneumonia, high dose glucocorticoids are recommended in the management of the patient. It is only anecdotal studies that suggest avoiding oxygen therapy in this condition. Bleomycin seems to exert its chemotherapeutic effect and pulmonary toxicity by forming complexes with oxygen, ferric Fe and inducing breaks in dsDNA (uptodate)
Question 2
What is the most common radiological pattern of lung involvement seen in patients with interstitial fibrosis secondary to connective tissue disease?
(A) Usual interstitial pneumonia
(B) Lymphocytic Interstitial Pneumonia
(C) Hypersensitivity pneumonitis pattern
(D) Non-specific Interstitial Pneumonia pattern
(E) Bronchiolitis obliterans organising pneumonia
D: UIP histology suggested by architectural distortion, patchy changes showing spatial and temporal heterogeneity and fibroblastic foci (pathognomonic) – RPA course, PEP lecture 2014
A: Prone HRCT is really only done in patients being investigated for IPF to showcase the early fibrotic changes. The sub-pleural septal and interlobular thickening with subpleural honeycombing is usually basal and posterior, therefore these changes are brought out by gravitational positioning in the prone position. Other radiological changes include sub-pleural honeycombing and traction bronchiectasis. Ground glass changes are seen in NSIP. Granulomas and upper lobe predominance is sarcoidosis, nodules is hypersensitivity pneumonitis (RPA lecture).
Question 4
What is the most important predictor of mortality in patients with idiopathic pulmonary fibrosis?
(A) DLCO
(B) 6MWT distance
(C) FVC drop of 10% in 6 months
(D) Age
(E) Male gender
C: According to PEP 2014 lecture
Question 5
What is the most common lung function test pattern seen in a patient with IPF?
(A) FEV1/ FVC <0.7, TLC >80% predicted, DLCO <80% but correctable for Va
(B) FEV1/ FVC >0.7, TLC <80% predicted, DLCO >80% but correctable for Va
(C) FEV1/ FVC >0.7, TLC >80% predicted, DLCO <80% but not-correctable for Va
(D) FEV1/ FVC >0.7, TLC <80% predicted, DLCO <80% but not-correctable for Va
(E) FEV1/ FVC >0.7, TLC <80% predicted, DLCO <80% but correctable for Va
E: Non-obstructive spirometry, restrictive lung volumes with reduced DLCO corrected for by alveolar volumes (PEP 2014, RPA course Dr Lauren Troy)
Question 6
In the ASCEND and CAPACITY trials looking at pirfenidone, what was the most common reported adverse event of pirfenidone compared to placebo?
(A) Insomnia
(B) Headache
(C) Rash
(D) Nausea
(E) Vomiting
D: Nausea was reported in 100% of patients. Other SE that were more commonly reported compared to placebo include Insomnia, rash and vomiting (1)
Question 7
Pooling the results of Pirfenidone trials in patients with IPF (ASCEND, CAPACITY 1 and CAPACITY 2), which of the following results is FALSE
(A) Decreased deaths (when pooled) related to Idiopathic pulmonary fibrosis
(B) Decreased deaths (when pooled) related to all cause mortality
(C) Reduction in decline of 6MWT
(D) Improvement in dyspnoea scores
(E) Reduction in decline of FVC
D:
Question 8
A 79 year old female from the country is referred to RPAH with pulmonary alveolar proteinosis secondary to JAK2 negative myelofibrosis. Her exercise tolerance has been gradually declining over the last year, however she has noticed a rapid decline in the last 3 weeks. She has reduced FEV1 compared to her baseline, and is coughing up more brown coloured sputum. With regards to her potential diagnosis, what is NOT an appropriate management step
(A) Admission for IV antibiotics for a presumed infective exacerbation of PAP
(B) Discussion with anaesthetics regarding whole lung lavage under ECMO support
(C) Pulse methylprednisolone and cyclophosphamide, with TMPT levels prior to azathioprine maintenance
(D) Intensive physiotherapy, hypertonic saline nebs and oxygen therapy to maintain saturations
(E) Optimising the management of her myelofibrosis
C: High dose immunosuppression has no role in this condition. Rare haematological conditions have been associated with PAP, an overall very rare disease in ILD clinics! Idiopathic PAP may be associated with antibodies to GM-CSF, and trials have generally been unyielding when patients with PAP have been given GM-CSF.
1. King TE, Jr., Bradford WZ, Castro-Bernardini S, Fagan EA, Glaspole I, Glassberg MK, et al. A phase 3 trial of pirfenidone in patients with idiopathic pulmonary fibrosis. N Engl J Med. 2014;370(22):2083-92.
Question 1:
A 38-year old garbage truck driver presents to the emergency department with one day of coughing paroxysms and a teaspoon of hemoptysis, which has since subsided. He reports no systemic features. His CXR shows bilateral upper lobe fibrosis with hilar lymphadenopathy. Clinically he saturates at 98% on room air without any evidence of respiratory distress. He was diagnosed in 2013 with sarcoid affecting the lungs and was commenced on a short term dose of tapering prednisolone of 40mg daily.
With regards to the treatment of sarcoidosis, what is LEAST correct?
(A) For 66% of patients, the natural history of sarcoidosis is for remission, with the remaining 33% suffering irreversible organ damage, with only 5% dying of sarcoidosis related complications (mainly respiratory failure)
(B) Hypercalciuria occurs in 40% of patients and is more common than Hypercalcaemia; the pathogenic substrate for the abnormalities relate to increased 1a hydroxylase activity.
(C) Cardiac sarcoid is usually a pathological entity found on autopsy, and effects the free left ventricular wall and interventricular septum
(D) Methotrexate has been shown to be steroid sparing in those patients that are steroid responsive and dependent
(E) This patient should be started on prednisolone 40mg daily as he has end organ failure
E: This patient does not show signs of end organ failure or life threatening organ involvement, and in any case a thorough search for alternative differential diagnosis should be sought after. The option would be different should the patient be in respiratory distress or severely hypoxic. Hypercalciuria is more common than hypercalcaemia, and should be offered to any patient with sarcoidosis. Biopsy is not necessary to diagnose sarcoid especially if they have the common syndrome of arthritis, erythema nodosum and hilar lymphadenopathy – Löfgren’s syndrome. Cardiac sarcoid, when it does occur, typically manifests with conduction delay or a cardiomyopathy secondary to loss of functional muscle tissue (1).
1. Iannuzzi MC, Rybicki BA, Teirstein AS. Sarcoidosis. N Engl J Med. 2007;357(21):2153-65.
A 38-year old garbage truck driver presents to the emergency department with one day of coughing paroxysms and a teaspoon of hemoptysis, which has since subsided. He reports no systemic features. His CXR shows bilateral upper lobe fibrosis with hilar lymphadenopathy. Clinically he saturates at 98% on room air without any evidence of respiratory distress. He was diagnosed in 2013 with sarcoid affecting the lungs and was commenced on a short term dose of tapering prednisolone of 40mg daily.
With regards to the treatment of sarcoidosis, what is LEAST correct?
(A) For 66% of patients, the natural history of sarcoidosis is for remission, with the remaining 33% suffering irreversible organ damage, with only 5% dying of sarcoidosis related complications (mainly respiratory failure)
(B) Hypercalciuria occurs in 40% of patients and is more common than Hypercalcaemia; the pathogenic substrate for the abnormalities relate to increased 1a hydroxylase activity.
(C) Cardiac sarcoid is usually a pathological entity found on autopsy, and effects the free left ventricular wall and interventricular septum
(D) Methotrexate has been shown to be steroid sparing in those patients that are steroid responsive and dependent
(E) This patient should be started on prednisolone 40mg daily as he has end organ failure
E: This patient does not show signs of end organ failure or life threatening organ involvement, and in any case a thorough search for alternative differential diagnosis should be sought after. The option would be different should the patient be in respiratory distress or severely hypoxic. Hypercalciuria is more common than hypercalcaemia, and should be offered to any patient with sarcoidosis. Biopsy is not necessary to diagnose sarcoid especially if they have the common syndrome of arthritis, erythema nodosum and hilar lymphadenopathy – Löfgren’s syndrome. Cardiac sarcoid, when it does occur, typically manifests with conduction delay or a cardiomyopathy secondary to loss of functional muscle tissue (1).
1. Iannuzzi MC, Rybicki BA, Teirstein AS. Sarcoidosis. N Engl J Med. 2007;357(21):2153-65.
Question 1:
Which of the following statements is FALSE regarding the diagnosis of mycobacterium tuberculosis?
(A) The IGRA test is the preferred test in diagnosing latent TB infection (LTBI) in patients who are immunosuppressed without HIV or in patients who have been vaccinated with BCG
(B) The IGRA test is better than the Mantoux test in diagnosing active TB
(C) The Mantoux test is cheaper than the IGRA test
(D) The proteins injected into the subcutis in the Mantoux test have reactivity with other non-tuberculous mycobacterium
(E) The IGRA test has higher false conversions from negative tests to positive tests and reversions from positive tests to negative tests in serially followed health workers than the Mantoux test
(F) Mycobacterium Kansasii reacts with the IGRA test, leading to false positive results.
(G) Mantoux test is preferable to IGRA in children <5y
B: It is important to note that IGRA or Mantoux can only be used to diagnose LTBI and has no role in diagnosing active TB. The main advantage of the IGRA test over the Mantoux test is that it doesn’t have cross-reactivity with BCG, therefore there is greater specificity in this group, and it may be used in patients who are immunosuppressed. Interestingly, IGRA does have a higher conversion and reversion rate in serially followed healthcare workers(1, 2). RPA lecture notes, Rebecca Davis 2015 were also used.
Question 2
A 68 year-old male who has rheumatoid arthritis with sero-positive erosive disease and raised inflammatory markers is undergoing consideration for biological therapies. Which of the following statements is TRUE regarding the use of the Mantoux test in this individual to screen for LTBI?
(A) The Mantoux test would not be as sensitive as the IGRA test given the patient is already immunosuppressed on non biological DMARDS, however a value of >5mm induration would support a diagnosis of LTBI
(B) The cut-off reading would be >5mm because we are expecting a lower immune response with immunosuppression
(C) The cut-off value would be >15mm because we want to increase specificity and treat only those that truly require prolonged course of toxic mycobacterial antibiotics.
(D) The cut-off would be >10mm as the patient falls in the intermediate pre-test probability region for diagnosis of LTBI
(E) The IGRA test should always be used over the Mantoux test and the level of positivity correlates with the risk of progression to active disease
(F) The IGRA test can be used to detect successful treatment
A: Mantoux test is important in the diagnosis of latent TB and is still recommended in Australia in most circumstances. The aim is to increase detection in the most susceptible groups (increase sensitivity perhaps at the expense of specificity) and thus the recommendation is >5mm should be the positive cut-off for patients who are immunosuppressed, who have had recent close exposure to patients with active TB and old TB as evidenced on chest radiography. >10 mm is the cut-off for nursing home residence, health care workers and foreign nationals born in TB endemic regions, with >15mm in BCG vaccinated patients and all other people. The level of positivity in the IGRA test correlates poorly to the risk of progression of active disease and should not be used as a predictor (1). Information also obtained from 2014 and 2015 PEP lecture.
Question 3
Which if the following biological agent is associated with the highest cumulative incidence of active TB?
(A) Infliximab
(B) Rituximab
(C) Ustekinumab
(D) adalimumab
(E) nilotanib
(F) etanercept
D: According to the 2014 PEP lecture, adalimumab is the biological agent (fully humanised TNF-alpha blocker) that is most associated with incidence of active TB. Infliximab has higher rates of TB incidence than does etanercept. Note rituximab is a risk factor for TB and guidelines require screening for latent TB in this group of patients.
Question 4
Which of the following age groups is at highest risk of developing TB disease in 2 years following TB exposure and infection
(A) Infants <1y
(B) Children 2 – 5y
(C) Children 5 – 10y
(D) Children 1 – 2y
(E) Older adults
(F) Adolescents
A: Infants <1y have a 50% risk of developing active TB after exposure, and are the highest age group at risk. Children aged 1 – 2y have a 12 – 25% risk, 2 – 5y have 5% risk, 5 – 10y have 2% risk, adolescents have 10 – 20% and elderly adults 3 – 5% risk (RPA TB and endocarditis lecture 2015, Dr Rebecca Davis)
Question 5
What is the CORRECT regime to be used in patients with latent TB infection?
(A) Isoniazid for 4 months
(B) Yearly CXR, and if progresses, treat with RIPE regime for 6 months
(C) Isoniazid for 6 – 9 months, or Rifampicin for 4 months
(D) Rifampicin, Isoniazid for 6 months, Rifampicin, Isoniazid, Vitamin B6, Pyrazinamide, Ethambutol for 2 months
(E) Amikacin, Rifampicin, levofloxacin for 4 months
C: Isoniazid for 6 – 9 months or Rifampicin for 4 months can be used to treat LTBI, reducing the risk of progression to active disease (RR 0.4). In some people, yearly CXR surveillance without treating if they are immunocompetent can be a reasonable strategy. If the patient is about to start treatment with anti-TNF alpha regimes then 6 – 8 weeks of pre-treatment with isoniazid is usually sufficient. S/E of isoniazid include peripheral neuropathy and hepatitis, therefore patients require vitamin B6 supplementation to prevent this effect (RPA Course 2015, RPA TB lecture Dr Rebecca Davis)(1).
Question 6
With regards to the mechanism of action of anti-TB drugs and potential side effects, what is FALSE?
(A) Rifampicin inhibits cell wall synthesis, works mainly against sporadically multiplying MTB, and side-effects include hepatotoxicity and potential drug interactions (CYP inducer)
(B) Isoniazid should be continued for 6 months of therapy, its actions are mainly on rapidly replicating pool of MTB, side effects include hepatitis and painful symmetrical peripheral neuropathy
(C) Ethambutol should be prescribed in the first 2 months, the main side effects are optic neuritis and its actions are on the rapidly multiplying pool of MTB
(D) Pyrazinamide is an agent that works on the slowly replicating pool of TB present in acidic caesuous granulomas and can cause rash, gout and hepatitis. It should be prescribed for 2 months
(E) Pyridoxine or vitamin B6 is especially important to prevent peripheral neuropathy in children taking isoniazid due to an exponential rise in neuropathy in this age group
E: Vitamin B6 does not have to be used in children; The reason is that it is mainly adults who have an exponential risk of peripheral neuropathy (RPA course 2015).
Question 7
A 78yo male patient presents from India with 4 months of fevers, night sweats and haemoptysis. He tells you that he has been visiting his aunt who has resistant TB. Which of the following defines a case of multi-drug resistant TB compared to XDR-TB?
(A) MDR TB has resistance to both rifampicin and isoniazid, XDR TB has resistance to Rifampicin + isoniazid + quinolone + injectable
(B) MDR TB has resistance to rifampicin, XDR TB has resistance to rifampicin and isoniazid
(C) MDR TB has resistance to rifampicin and isoniazid, XDR TB has resistance to rifampicin, isoniazid, pyrazinamide and ethambutol
(D) MDR TB has resistance to rifampicin and isoniazid, XDR TB has resistance to rifampicin, isoniazid, pyrazinamide and ethambutol plus a quinolone
(E) MDR TB has resistance to isoniazid XDR TB has resistance to rifampicin and isoniazid
A: This is the case definition of MDR TB and XDR TB, PCR testing can be done, followed by culture for confirmation (3). Isoniazid resistance is the most common, followed by rifampicin resistance. There is a high chance of developing drug resistance if one drug is added to a failing regime. The hot spots for MDR include India, China and the ex-soviet region. Treatment includes prolonging the length to at least 18 – 24 months, adding a quinolone and an injectable. MDR usually develops in the course of failed therapy and transmission is usually less because of reduced transmissibility.
Question 8
In multi-drug resistant TB, the diarylquinoline bedaquiline has been used for multidrug resistant TB as it has been shown to accelerate the rate of sputum conversion. The addition of bedaquiline to a suitable background regime achieved what following outcome in a recent NEJM trial
(A) Decreased rate of culture conversion
(B) Increased deaths
(C) Decreased morbidity
(D) Intractable hypermagnesaemia
(E) hyperammonemic encephalopathy
B. According to a 2014 publication, there was greater sputum culture conversion however there were more deaths (10 compared to 2) in the bedaquiline + background group compared to background + placebo. The cause of the deaths was unknown, interestingly the adverse event rates were similar in both groups (4).
Question 10
A 51 year old male with bulls pemphigoid presents to the TB clinic referred from the dermatology clinic with a positive quanteferon gold test. The positive titre is >4 (>0.35 is significant). The dermatology team want to initiate the patient on mycophenylate as a steroid sparing agent but are worried about the effect of immunosuppression. On further questioning the patient has had previously treated TB as a child. He cannot remember the details of the treatment.
What is the best management approach
(A) Offer isoniazid + vitamin B6 as patient is high risk for having latent TB and will undergo immunosuppressant therapy with high risk medication. Inform dermatology team to delay immunosuppression for one month
(B) offer rifampicin in order to shorten the duration of therapy
(C) offer yearly follow up chest x-rays as part of the TB surveillance program
(D) Discharge patient from clinic
(E) Offer isoniazid + vitamin B6 as patient is high risk for having latent TB and will undergo immunosuppressant therapy with high risk medication. Inform dermatology that they cannot prescribe further immunosuppressants as patient is at extremely high risk of sputum conversion
A: This patient requires therapy as he is at high risk for sputum conversion. Isoniazid is generally well accepted and treatment is for 9 months at a dose of 300mg daily. Vitamin B6 is offered at 25mg daily. He should have monthly LFTs done and have 3 monthly follow up appointments at the TB clinic. If he is compliant, then the length can be prolonged between clinic visits. Rifampicin for 6 months is also a valid option however is not considered first line. Yearly CXRs are offered to patients with low risk of sputum conversion. The patients main concern is his blistering skin condition not his TB therefore immunosuppression should be continued. If the patient was to be started on azathioprine or methotrexate then the patient can start isoniazid + pyridoxine in concert with these agents. RPA TB clinic information guidelines
Question 11
A 26 year old female nurse presents to the TB clinic following a positive exposure to TB. She has never been previously exposed. An initial mantoux test shows an induration of 3mm. She is also quantaferon negative. What is the most appropriate step?
(A) offer her post-exposure prophylaxis
(B) discharge her with reassurance
(C) Offer her a CXR and repeat quantaferon/ mantoux test in one months time, and follow her up, looking for conversion
(D) Offer her treatment as per LTBI
(E) Offer her a CXR and only treat her if her CXR becomes positive.
C: This patient has documented TB exposure and no active infection. Furthermore she is not immunosuppressed, therefore it would be important to repeat the TST or mantoux test in her as these can take a while to convert to positive. Should she convert to positive then there is sufficient evidence to support a diagnosis of LTBI, and consideration should be given to INH versus CXR follow up, usually for a period of 2 - 3 years.
Question 12
What is true regarding the pharmacokinetics of isoniazid treatment?
(A) Fast acetylators (N-acetyltransferase) have higher rates of hepatotoxicity
(B) Slow acetylators (N-acetyltransferase) have higher rates of hepatotoxicity
(C) Fast acetylators (N-acetyltransferase) have lower rates of pulmonary fibrosis
(D) Hepatotoxicity is normally cholestatic
(E) Polyneuropathy or neurotoxicity is a rare side effect
B: N-acetyltransferase is an enzyme that is involved in isoniazid clearance; human genetic variation in the gene encoding N-acetyltransferase (NAT2) can lead to underexposure (in “fast acetylators”) or to an elevated risk of hepatotoxicity (in “slow acetylators”); this slow-acetylator genotype is present in more than 50% of white populations N Engl J Med 2015; 373:2149-2160.
Question 13
What is FALSE regarding the toxicity of rifampicin
(A) Can cause haemolytic anaemia
(B) It is a potent enzyme inducer
(C) can cause a cholestatic hepatotoxicity
(D) Can cause discolouration of human body fluids
(E) Has a high rate of interstitial pneumonitis
E: N Engl J Med 2015; 373:2149-2160.
1. Getahun H, Chaisson RE, Raviglione M. Latent Mycobacterium tuberculosis Infection. N Engl J Med. 2015;373(12):1179-80.
2. Dorman SE, Belknap R, Graviss EA, Reves R, Schluger N, Weinfurter P, et al. Interferon-gamma release assays and tuberculin skin testing for diagnosis of latent tuberculosis infection in healthcare workers in the United States. Am J Respir Crit Care Med. 2014;189(1):77-87.
3. Millard J, Ugarte-Gil C, Moore DA. Multidrug resistant tuberculosis. BMJ. 2015;350:h882.
4. Diacon AH, Pym A, Grobusch MP, de los Rios JM, Gotuzzo E, Vasilyeva I, et al. Multidrug-resistant tuberculosis and culture conversion with bedaquiline. N Engl J Med. 2014;371(8):723-32.
Which of the following statements is FALSE regarding the diagnosis of mycobacterium tuberculosis?
(A) The IGRA test is the preferred test in diagnosing latent TB infection (LTBI) in patients who are immunosuppressed without HIV or in patients who have been vaccinated with BCG
(B) The IGRA test is better than the Mantoux test in diagnosing active TB
(C) The Mantoux test is cheaper than the IGRA test
(D) The proteins injected into the subcutis in the Mantoux test have reactivity with other non-tuberculous mycobacterium
(E) The IGRA test has higher false conversions from negative tests to positive tests and reversions from positive tests to negative tests in serially followed health workers than the Mantoux test
(F) Mycobacterium Kansasii reacts with the IGRA test, leading to false positive results.
(G) Mantoux test is preferable to IGRA in children <5y
B: It is important to note that IGRA or Mantoux can only be used to diagnose LTBI and has no role in diagnosing active TB. The main advantage of the IGRA test over the Mantoux test is that it doesn’t have cross-reactivity with BCG, therefore there is greater specificity in this group, and it may be used in patients who are immunosuppressed. Interestingly, IGRA does have a higher conversion and reversion rate in serially followed healthcare workers(1, 2). RPA lecture notes, Rebecca Davis 2015 were also used.
Question 2
A 68 year-old male who has rheumatoid arthritis with sero-positive erosive disease and raised inflammatory markers is undergoing consideration for biological therapies. Which of the following statements is TRUE regarding the use of the Mantoux test in this individual to screen for LTBI?
(A) The Mantoux test would not be as sensitive as the IGRA test given the patient is already immunosuppressed on non biological DMARDS, however a value of >5mm induration would support a diagnosis of LTBI
(B) The cut-off reading would be >5mm because we are expecting a lower immune response with immunosuppression
(C) The cut-off value would be >15mm because we want to increase specificity and treat only those that truly require prolonged course of toxic mycobacterial antibiotics.
(D) The cut-off would be >10mm as the patient falls in the intermediate pre-test probability region for diagnosis of LTBI
(E) The IGRA test should always be used over the Mantoux test and the level of positivity correlates with the risk of progression to active disease
(F) The IGRA test can be used to detect successful treatment
A: Mantoux test is important in the diagnosis of latent TB and is still recommended in Australia in most circumstances. The aim is to increase detection in the most susceptible groups (increase sensitivity perhaps at the expense of specificity) and thus the recommendation is >5mm should be the positive cut-off for patients who are immunosuppressed, who have had recent close exposure to patients with active TB and old TB as evidenced on chest radiography. >10 mm is the cut-off for nursing home residence, health care workers and foreign nationals born in TB endemic regions, with >15mm in BCG vaccinated patients and all other people. The level of positivity in the IGRA test correlates poorly to the risk of progression of active disease and should not be used as a predictor (1). Information also obtained from 2014 and 2015 PEP lecture.
Question 3
Which if the following biological agent is associated with the highest cumulative incidence of active TB?
(A) Infliximab
(B) Rituximab
(C) Ustekinumab
(D) adalimumab
(E) nilotanib
(F) etanercept
D: According to the 2014 PEP lecture, adalimumab is the biological agent (fully humanised TNF-alpha blocker) that is most associated with incidence of active TB. Infliximab has higher rates of TB incidence than does etanercept. Note rituximab is a risk factor for TB and guidelines require screening for latent TB in this group of patients.
Question 4
Which of the following age groups is at highest risk of developing TB disease in 2 years following TB exposure and infection
(A) Infants <1y
(B) Children 2 – 5y
(C) Children 5 – 10y
(D) Children 1 – 2y
(E) Older adults
(F) Adolescents
A: Infants <1y have a 50% risk of developing active TB after exposure, and are the highest age group at risk. Children aged 1 – 2y have a 12 – 25% risk, 2 – 5y have 5% risk, 5 – 10y have 2% risk, adolescents have 10 – 20% and elderly adults 3 – 5% risk (RPA TB and endocarditis lecture 2015, Dr Rebecca Davis)
Question 5
What is the CORRECT regime to be used in patients with latent TB infection?
(A) Isoniazid for 4 months
(B) Yearly CXR, and if progresses, treat with RIPE regime for 6 months
(C) Isoniazid for 6 – 9 months, or Rifampicin for 4 months
(D) Rifampicin, Isoniazid for 6 months, Rifampicin, Isoniazid, Vitamin B6, Pyrazinamide, Ethambutol for 2 months
(E) Amikacin, Rifampicin, levofloxacin for 4 months
C: Isoniazid for 6 – 9 months or Rifampicin for 4 months can be used to treat LTBI, reducing the risk of progression to active disease (RR 0.4). In some people, yearly CXR surveillance without treating if they are immunocompetent can be a reasonable strategy. If the patient is about to start treatment with anti-TNF alpha regimes then 6 – 8 weeks of pre-treatment with isoniazid is usually sufficient. S/E of isoniazid include peripheral neuropathy and hepatitis, therefore patients require vitamin B6 supplementation to prevent this effect (RPA Course 2015, RPA TB lecture Dr Rebecca Davis)(1).
Question 6
With regards to the mechanism of action of anti-TB drugs and potential side effects, what is FALSE?
(A) Rifampicin inhibits cell wall synthesis, works mainly against sporadically multiplying MTB, and side-effects include hepatotoxicity and potential drug interactions (CYP inducer)
(B) Isoniazid should be continued for 6 months of therapy, its actions are mainly on rapidly replicating pool of MTB, side effects include hepatitis and painful symmetrical peripheral neuropathy
(C) Ethambutol should be prescribed in the first 2 months, the main side effects are optic neuritis and its actions are on the rapidly multiplying pool of MTB
(D) Pyrazinamide is an agent that works on the slowly replicating pool of TB present in acidic caesuous granulomas and can cause rash, gout and hepatitis. It should be prescribed for 2 months
(E) Pyridoxine or vitamin B6 is especially important to prevent peripheral neuropathy in children taking isoniazid due to an exponential rise in neuropathy in this age group
E: Vitamin B6 does not have to be used in children; The reason is that it is mainly adults who have an exponential risk of peripheral neuropathy (RPA course 2015).
Question 7
A 78yo male patient presents from India with 4 months of fevers, night sweats and haemoptysis. He tells you that he has been visiting his aunt who has resistant TB. Which of the following defines a case of multi-drug resistant TB compared to XDR-TB?
(A) MDR TB has resistance to both rifampicin and isoniazid, XDR TB has resistance to Rifampicin + isoniazid + quinolone + injectable
(B) MDR TB has resistance to rifampicin, XDR TB has resistance to rifampicin and isoniazid
(C) MDR TB has resistance to rifampicin and isoniazid, XDR TB has resistance to rifampicin, isoniazid, pyrazinamide and ethambutol
(D) MDR TB has resistance to rifampicin and isoniazid, XDR TB has resistance to rifampicin, isoniazid, pyrazinamide and ethambutol plus a quinolone
(E) MDR TB has resistance to isoniazid XDR TB has resistance to rifampicin and isoniazid
A: This is the case definition of MDR TB and XDR TB, PCR testing can be done, followed by culture for confirmation (3). Isoniazid resistance is the most common, followed by rifampicin resistance. There is a high chance of developing drug resistance if one drug is added to a failing regime. The hot spots for MDR include India, China and the ex-soviet region. Treatment includes prolonging the length to at least 18 – 24 months, adding a quinolone and an injectable. MDR usually develops in the course of failed therapy and transmission is usually less because of reduced transmissibility.
Question 8
In multi-drug resistant TB, the diarylquinoline bedaquiline has been used for multidrug resistant TB as it has been shown to accelerate the rate of sputum conversion. The addition of bedaquiline to a suitable background regime achieved what following outcome in a recent NEJM trial
(A) Decreased rate of culture conversion
(B) Increased deaths
(C) Decreased morbidity
(D) Intractable hypermagnesaemia
(E) hyperammonemic encephalopathy
B. According to a 2014 publication, there was greater sputum culture conversion however there were more deaths (10 compared to 2) in the bedaquiline + background group compared to background + placebo. The cause of the deaths was unknown, interestingly the adverse event rates were similar in both groups (4).
Question 10
A 51 year old male with bulls pemphigoid presents to the TB clinic referred from the dermatology clinic with a positive quanteferon gold test. The positive titre is >4 (>0.35 is significant). The dermatology team want to initiate the patient on mycophenylate as a steroid sparing agent but are worried about the effect of immunosuppression. On further questioning the patient has had previously treated TB as a child. He cannot remember the details of the treatment.
What is the best management approach
(A) Offer isoniazid + vitamin B6 as patient is high risk for having latent TB and will undergo immunosuppressant therapy with high risk medication. Inform dermatology team to delay immunosuppression for one month
(B) offer rifampicin in order to shorten the duration of therapy
(C) offer yearly follow up chest x-rays as part of the TB surveillance program
(D) Discharge patient from clinic
(E) Offer isoniazid + vitamin B6 as patient is high risk for having latent TB and will undergo immunosuppressant therapy with high risk medication. Inform dermatology that they cannot prescribe further immunosuppressants as patient is at extremely high risk of sputum conversion
A: This patient requires therapy as he is at high risk for sputum conversion. Isoniazid is generally well accepted and treatment is for 9 months at a dose of 300mg daily. Vitamin B6 is offered at 25mg daily. He should have monthly LFTs done and have 3 monthly follow up appointments at the TB clinic. If he is compliant, then the length can be prolonged between clinic visits. Rifampicin for 6 months is also a valid option however is not considered first line. Yearly CXRs are offered to patients with low risk of sputum conversion. The patients main concern is his blistering skin condition not his TB therefore immunosuppression should be continued. If the patient was to be started on azathioprine or methotrexate then the patient can start isoniazid + pyridoxine in concert with these agents. RPA TB clinic information guidelines
Question 11
A 26 year old female nurse presents to the TB clinic following a positive exposure to TB. She has never been previously exposed. An initial mantoux test shows an induration of 3mm. She is also quantaferon negative. What is the most appropriate step?
(A) offer her post-exposure prophylaxis
(B) discharge her with reassurance
(C) Offer her a CXR and repeat quantaferon/ mantoux test in one months time, and follow her up, looking for conversion
(D) Offer her treatment as per LTBI
(E) Offer her a CXR and only treat her if her CXR becomes positive.
C: This patient has documented TB exposure and no active infection. Furthermore she is not immunosuppressed, therefore it would be important to repeat the TST or mantoux test in her as these can take a while to convert to positive. Should she convert to positive then there is sufficient evidence to support a diagnosis of LTBI, and consideration should be given to INH versus CXR follow up, usually for a period of 2 - 3 years.
Question 12
What is true regarding the pharmacokinetics of isoniazid treatment?
(A) Fast acetylators (N-acetyltransferase) have higher rates of hepatotoxicity
(B) Slow acetylators (N-acetyltransferase) have higher rates of hepatotoxicity
(C) Fast acetylators (N-acetyltransferase) have lower rates of pulmonary fibrosis
(D) Hepatotoxicity is normally cholestatic
(E) Polyneuropathy or neurotoxicity is a rare side effect
B: N-acetyltransferase is an enzyme that is involved in isoniazid clearance; human genetic variation in the gene encoding N-acetyltransferase (NAT2) can lead to underexposure (in “fast acetylators”) or to an elevated risk of hepatotoxicity (in “slow acetylators”); this slow-acetylator genotype is present in more than 50% of white populations N Engl J Med 2015; 373:2149-2160.
Question 13
What is FALSE regarding the toxicity of rifampicin
(A) Can cause haemolytic anaemia
(B) It is a potent enzyme inducer
(C) can cause a cholestatic hepatotoxicity
(D) Can cause discolouration of human body fluids
(E) Has a high rate of interstitial pneumonitis
E: N Engl J Med 2015; 373:2149-2160.
1. Getahun H, Chaisson RE, Raviglione M. Latent Mycobacterium tuberculosis Infection. N Engl J Med. 2015;373(12):1179-80.
2. Dorman SE, Belknap R, Graviss EA, Reves R, Schluger N, Weinfurter P, et al. Interferon-gamma release assays and tuberculin skin testing for diagnosis of latent tuberculosis infection in healthcare workers in the United States. Am J Respir Crit Care Med. 2014;189(1):77-87.
3. Millard J, Ugarte-Gil C, Moore DA. Multidrug resistant tuberculosis. BMJ. 2015;350:h882.
4. Diacon AH, Pym A, Grobusch MP, de los Rios JM, Gotuzzo E, Vasilyeva I, et al. Multidrug-resistant tuberculosis and culture conversion with bedaquiline. N Engl J Med. 2014;371(8):723-32.
Question 1
A 32 year-old patient with left calf swelling who is 12 weeks gestation with her pregnancy attends her routine antenatal class. Keeping in mind the most likely diagnosis, what is the LEAST correct option
(A) Duplex ultrasound has high negative predictive value, therefore a negative test will help rule out a deep vein thrombosis
(B) The left leg is the most common site affected by DVT in the setting of pregnancy
(C) The risk of DVT is greatest in the first 20 weeks and then 6 weeks (up to three months in some studies) post-partum, therefore anticoagulation should be continued until at least this time
(D) Deep vein thrombosis occurs mainly in the third trimester when patients are naturally most immobile and the bodies anti-fibrinolytic system is unregulated to protect the placenta from micro-thrombosis
(E) Warfarin is contra-indicated in this setting in comparison to low molecular weight heparin because of the risks of teratogenicity and increased bleeding risks to the foetus
D: DVT is greatest in the first 20 weeks (accounts for 50%) and then 6 weeks thereafter (1). Note that uptodate says that the highest risk is postpartum and that all trimesters are affected in equal proportions. Using MCQ techniques one would know the answer is either C or D as neither can be correct at the same time. 85% of the time the left leg is affected compared to 55% in non-pregnant females, and is thought to be brought on by compression of the left iliac vein by the right iliac artery (2). The mechanism of pro-thrombosis in pregnancy probably relates to a combination of stasis, endothelial injury especially in the immediate post-partum state and hyper-coaguability (increase in several coagulation factors and decrease in protein S with high protein C resistance (3)
Question 2
Which of these is the STRONGEST risk factor for VTE in pregnancy?
(A) Previous VTE in pregnancy
(B) Prothrombin mutation
(C) Factor V Leiden mutation
(D) Previous use of the combined oral contraceptive pill
(E) BMI >30
A: Thrombophilias, high BMI are all positively associated with VTE risk in pregnancy, but the highest risk is if a thrombosis has occurred in the past pregnancy. The risk of recurrence if one has had a previous VTE is estimated to be 6 – 9% (4).
Question 3
With regards to the diagnosis of VTE in pregnancy, which statement is INCORRECT?
(A) If pulmonary embolus is suspected based on clinical history, chest imaging is NOT required if there is clear evidence of a proximal DVT
(B) V/Q scan is the preferred imaging modality in pregnancy provided that there are no abnormal chest findings because of the decreased radiation exposure to maternal breast tissue
(C) D-Dimer should NOT be used in diagnostic algorithms concerning PE and pregnant women
(D) The traditional Wells criterion is NOT validated for its use in guiding further investigations in pregnant women
(E) CTPA exposes the pregnant foetus to greater radiation than does the V/Q scan
E: It is a myth that CTPA exposes the gravid foetus to radiation of significance. The dose estimated is 0.1 mGy, comparable to V/Q scanning (0.5 mGy) and are well below the values associated with teratogenicity (5). The reason that V/Q scanning is preferred is due to the fact that there is unlikely going to be chest abnormalities in a young population that would otherwise hinder interpretation (indeterminate result). The ventilation portion of the scan can also be omitted if required. CTPA exposes maternal breast tissue to 20 mGy radiation dose, with a small concern for breast cancer. This can be mitigated by wearing breast shields (40% reduction in radiation exposure).
Question 4
A 32-year-old G1P0 6/40 gestation presents with left calf swelling. She has an elective cesarian section booked for her delivery. Duplex venography confirms a non-compressible vessel extending into the common femoral vein. With regards to the best treatment, what would you advice?
(A) Immediate BD or OD LMWH starting from diagnosis and extending to 6 weeks post-partum, switching over to warfarin therapy post-partum. Withhold anti-coagulation 24 hours prior to neuroaxial anaesthesia and then 4 hours after removal of the epidural catheter to minimise risk of epidural haematoma
(B) Initiate warfarin low dose 3mg after LMWH bridging and continue warfarin indefinitely afterwards
(C) Initiate BD or OD LMWH starting from diagnosis and extending 3 months post-partum, switching over to warfarin therapy post-partum. Withhold anti-coagulation 24 hours prior to neuroaxial anaesthesia and then 4 hours after removal of the epidural catheter to minimise risk of epidural haematoma
(D) Start UFH given the unknown risks associated with LMWH to the foetus and better monitoring. Continue until 6 weeks post-partum
(E) Immediate BD or OD LMWH starting from diagnosis and extending to 6 weeks post-partum, switching over to warfarin therapy post-partum. Withhold anti-coagulation 8 hours prior to neuroaxial anaesthesia and then 2 hours after removal of the epidural catheter to minimise risk of epidural haematoma
A: This is the advice given by the NEJM article. Warfarin is contra-indicated in this setting, even though the dose is low. Furthermore, it is presumptuous to assume that 3mg of warfarin is the correct dose for the patient. Warfarin will be able to be commenced postpartum as it only minimally crosses into breast milk. NOACS should be avoided as it has not been validated in this setting. These agents may cross the placenta and have adverse fetal outcomes.
1. Greer IA. CLINICAL PRACTICE. Pregnancy Complicated by Venous Thrombosis. N Engl J Med. 2015;373(6):540-7.
2. Bourjeily G, Paidas M, Khalil H, Rosene-Montella K, Rodger M. Pulmonary embolism in pregnancy. Lancet. 2010;375(9713):500-12.
3. Walker MC, Garner PR, Keely EJ, Rock GA, Reis MD. Changes in activated protein C resistance during normal pregnancy. Am J Obstet Gynecol. 1997;177(1):162-9.
4. Bates SM, Greer IA, Middeldorp S, Veenstra DL, Prabulos AM, Vandvik PO, et al. VTE, thrombophilia, antithrombotic therapy, and pregnancy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e691S-736S.
5. Schembri GP, Miller AE, Smart R. Radiation dosimetry and safety issues in the investigation of pulmonary embolism. Semin Nucl Med. 2010;40(6):442-54.
Question 1: Epidemiology (1)
A 69 year-old male with progressive breathlessness is admitted under the medical assessment and planning unit (MAPU) with progressive breathlessness for investigation. He had an unprovoked pulmonary embolus 3 years ago that was treated with 6 months of warfarin. Since that time, he has noted his breathlessness to worsen progressively. Further complaints include intermittent dizziness and syncope. He has noted an increase in his abdominal girth with accompanying leg swelling. He is now largely bed-bound and is completely dependent on his family for his activities of daily living. He has a loud P2, an ejection systolic murmur over the tricuspid region and a right ventricular heave. His JVP is elevated without ‘a’ waves but prominent ‘v’ waves. He has shifting dullness and peripheral oedema up to mid thigh. His ECG shows signs of right ventricular hypertrophy, and his ECHO estimates a systolic pulmonary pressure of 55mmHg using the estimated tricuspid jet velocity in ‘M’ mode.
With regards to his most likely diagnosis, what is the most CORRECT statement?
(A) Idiopathic pulmonary arterial hypertension (IPAH) patients most likely carry the mutation for Bone Morphogenetic Receptor 2
(B) The expected survival of a patient who responds to inhaled nitric oxide with a drop in their mean pulmonary arterial pressure of 8mmHg is highly favourable if they are placed on high dose nifedipine or diltiazem
(C) 10% of patients will get pulmonary hypertension complicating a pulmonary embolus
(D) The treatment of patients with pulmonary artery hypertension secondary to obesity hypoventilation syndrome is similar to that of pulmonary artery hypertension secondary to chronic thromboembolic disease
(E) The mean age of diagnosis if idiopathic pulmonary arterial hypertension (IPAH) is 55 years with a median survival that is improving, however 5 year survival being only 2.8 years
Question 2: Epidemiology and prognostic factors
Which of these following factors is NOT a known adverse prognostic feature of pulmonary arterial hypertension
(A) Echocardiographic findings of large right atrial diameter, diastolic septal shifting and pericardial effusions
(B) Hypocapnia
(C) ECG findings of atrial fibrillation, atrial flutter or prolonged QRS duration
(D) Female gender
(E) Six minute walk test
Question 3: Clinical Diagnosis
On the Jugular venous pressure trace, what feature is associated with pulmonary arterial hypertension?
(A) Absent ‘a’ waves
(B) Prolonged ‘x’ and ‘y’ descent
(C) Kausmalls sign
(D) Cannon ‘a’ waves
(E) Raised ‘v’ waves
Question 4: Clinical Diagnosis
Which of the following clinical signs are NOT associated with pulmonary arterial hypertension?
(A) Right ventricular lift
(B) Pulsatile liver, ascites and peripheral oedema
(C) Early decrescendo diastolic murmur with pre-systolic blowing murmur
(D) Right ventricular third heart sound
(E) Paradoxically split second heart sound with palpable S2
Question 5: Clinical Diagnosis
What is the most common arrhythmia associated with pulmonary arterial hypertension?
(A) Atrial Fibrillation
(B) Atrial Flutter
(C) Atrio-Ventricular Nodal Re-entrant Tachycardia
(D) Idioventricular Rhythm
(E) Sinus Bradycardia
Question 6: Clinical Diagnosis
A 69 year-old male with progressive breathlessness is admitted under the medical assessment and planning unit (MAPU) with progressive breathlessness for investigation. He had an unprovoked pulmonary embolus 3 years ago that was treated with 6 months of warfarin. Since that time, he has noted his breathlessness to worsen progressively. Further complaints include intermittent dizziness and syncope. He has noted an increase in his abdominal girth with accompanying leg swelling. He is now largely bed-bound and is completely dependent on his family for his activities of daily living. He has a loud P2, an ejection systolic murmur over the tricuspid region and a right ventricular heave. His JVP is elevated without ‘a’ waves but prominent ‘v’ waves. He has shifting dullness and peripheral oedema up to mid thigh. His ECG shows signs of right ventricular hypertrophy, and his ECHO estimates a systolic pulmonary pressure of 55mmHg using the estimated tricuspid jet velocity in ‘M’ mode.
What chest X-ray imaging sign would be LEAST associated with pulmonary hypertension
(A) Cardiomegaly
(B) Pulmonary Arterial Pruning
(C) Right Upper Lobe consolidation with air-bronchograms
(D) Bi-basal predominant interstitial infiltrates resembling fibrosis
(E) Hampton’s hump
Question 7: Clinical Diagnosis
A 28 year-old man is suspected of having idiopathic pulmonary artery hypertension with a JVP measuring 5cm above sternal notch. He has an echocardiogram performed. The views were of sufficient quality, enabling the sonographer to calculate the following parameters:
Tricuspid regurgitant jet velocity: 4m.s-1
Left ventricular Ejection Fraction using Simpsons Method: 58%
Fractional shortening: 37%
What is the BEST fit for calculated parameters of Pressure gradient (dP), Right atrial Pressure, Systolic Pressure and Diagnosis
Answer
(A) Pressure gradient (dP) 64, RAP 10, sPAP 54, Diagnosis: Pulmonary hypertension
(B) Pressure gradient (dP)64, RAP 10, sPAP 74, Diagnosis: Undetermined
(C) Pressure gradient (dP) 64, RAP 5, sPAP 69, Diagnosis: Undetermined
(D) Pressure gradient (dP) 48, RAP 5, sPAP 53, Diagnosis: Pulmonary Hypertension
(E) Pressure gradient (dP) 48, RAP 10, sPAP 58, Diagnosis: Pulmonary Hypertension
Question 9: Categories of pulmonary hypertension
Once the diagnosis of pulmonary arterial hypertension is distinguished from pulmonary venous hypertension, which of the below options does NOT adequately help distinguish a cause
(A) ANA and interstitial lung disease
(B) V/Q and CTPEH
(C) anti-scl70 and diffuse scleroderma
(D) anti-centromere and limited scleroderma
(E) HIV third generation antigen/ antibody and HIV
Question 10: Causes
Which of the following medications are NOT associated with idiopathic pulmonary arterial hypertension
(A) dasatinib
(B) appetite suppressants
(C) St Johns wort
(D) chronic cocaine use
(E) obinutuzumab
Question 11: Treatment
A 68 year-old male with idiopathic pulmonary hypertension is undergoing consideration for treatment. Which of the following statements is FALSE about the role of anti-coagulation.
(A) Warfarin is the anticoagulation of choice because other studies are lacking
(B) A meta-analysis of seven observational studies has shown a benefit favouring anti-coagulation in terms of mortality
(C) There is no difference in bleeding risk in patients with PAH secondary to connective tissue disease in comparison to patients with idiopathic pulmonary hypertension
(D) There is no evidence for use of anticoagulation in PAH due to anorexigens
(E) The rationale for anti-coagulation is due to sluggish pulmonary blood flow leading to a predisposition for thrombosis on the background of poor physiological reserve
Question 12: Treatment
Which patient group is most likely to respond to the nitrous oxide vasoreactivity test?
(A) Pulmonary arterial hypertension secondary to non-specific interstitial pneumonia
(B) Pulmonary arterial hypertension secondary to drugs such as anorexigen
(C) Pulmonary arterial hypertension secondary to HIV
(D) Pulmonary arterial hypertension secondary to schistosomiasis
(E) Pulmonary arterial hypertension secondary to PTPN22a mutation
Question 13: Treatment
What is the mortality of a patient who has pulmonary arterial hypertension who falls pregnant?
(A) 17 – 33%
(B) 2 – 12%
(C) 35 – 60%
(D) 50 – 70%
(E) 60 – 85%
Question 14: Treatment
Which of the following statements is INCORRECT
(A) Bosentan and ambrisentan are endothelin receptor antagonists, functionally causing a pulmonary vasodilated state, with Bosentan causing reversible liver function abnormalities in 10% requiring monthly LFT monitoring
(B) Sildanefil and tadalafil inhibit phosphodiesterase 5, which causes increased cyclic GMP via nitrous oxide therefore causing pulmonary smooth muscle vasodilation. Its use is contra-indicated with other nitrates
(C) One criterion of the PBS states that right heart catheterisation should be used and the criterion is that the mean pulmonary arterial pressure is greater than 25 mmHg with the pulmonary capillary wedge pressure less than 15mmHg
(D) Prostanoids are prostacyclins that cause pulmonary arterial vasodilation with added anti-proliferative effects
(E) Riociguat cannot be used for the treatment of pulmonary artery hypertension secondary to chronic thromboembolic disease
A 69 year-old male with progressive breathlessness is admitted under the medical assessment and planning unit (MAPU) with progressive breathlessness for investigation. He had an unprovoked pulmonary embolus 3 years ago that was treated with 6 months of warfarin. Since that time, he has noted his breathlessness to worsen progressively. Further complaints include intermittent dizziness and syncope. He has noted an increase in his abdominal girth with accompanying leg swelling. He is now largely bed-bound and is completely dependent on his family for his activities of daily living. He has a loud P2, an ejection systolic murmur over the tricuspid region and a right ventricular heave. His JVP is elevated without ‘a’ waves but prominent ‘v’ waves. He has shifting dullness and peripheral oedema up to mid thigh. His ECG shows signs of right ventricular hypertrophy, and his ECHO estimates a systolic pulmonary pressure of 55mmHg using the estimated tricuspid jet velocity in ‘M’ mode.
With regards to his most likely diagnosis, what is the most CORRECT statement?
(A) Idiopathic pulmonary arterial hypertension (IPAH) patients most likely carry the mutation for Bone Morphogenetic Receptor 2
(B) The expected survival of a patient who responds to inhaled nitric oxide with a drop in their mean pulmonary arterial pressure of 8mmHg is highly favourable if they are placed on high dose nifedipine or diltiazem
(C) 10% of patients will get pulmonary hypertension complicating a pulmonary embolus
(D) The treatment of patients with pulmonary artery hypertension secondary to obesity hypoventilation syndrome is similar to that of pulmonary artery hypertension secondary to chronic thromboembolic disease
(E) The mean age of diagnosis if idiopathic pulmonary arterial hypertension (IPAH) is 55 years with a median survival that is improving, however 5 year survival being only 2.8 years
Question 2: Epidemiology and prognostic factors
Which of these following factors is NOT a known adverse prognostic feature of pulmonary arterial hypertension
(A) Echocardiographic findings of large right atrial diameter, diastolic septal shifting and pericardial effusions
(B) Hypocapnia
(C) ECG findings of atrial fibrillation, atrial flutter or prolonged QRS duration
(D) Female gender
(E) Six minute walk test
Question 3: Clinical Diagnosis
On the Jugular venous pressure trace, what feature is associated with pulmonary arterial hypertension?
(A) Absent ‘a’ waves
(B) Prolonged ‘x’ and ‘y’ descent
(C) Kausmalls sign
(D) Cannon ‘a’ waves
(E) Raised ‘v’ waves
Question 4: Clinical Diagnosis
Which of the following clinical signs are NOT associated with pulmonary arterial hypertension?
(A) Right ventricular lift
(B) Pulsatile liver, ascites and peripheral oedema
(C) Early decrescendo diastolic murmur with pre-systolic blowing murmur
(D) Right ventricular third heart sound
(E) Paradoxically split second heart sound with palpable S2
Question 5: Clinical Diagnosis
What is the most common arrhythmia associated with pulmonary arterial hypertension?
(A) Atrial Fibrillation
(B) Atrial Flutter
(C) Atrio-Ventricular Nodal Re-entrant Tachycardia
(D) Idioventricular Rhythm
(E) Sinus Bradycardia
Question 6: Clinical Diagnosis
A 69 year-old male with progressive breathlessness is admitted under the medical assessment and planning unit (MAPU) with progressive breathlessness for investigation. He had an unprovoked pulmonary embolus 3 years ago that was treated with 6 months of warfarin. Since that time, he has noted his breathlessness to worsen progressively. Further complaints include intermittent dizziness and syncope. He has noted an increase in his abdominal girth with accompanying leg swelling. He is now largely bed-bound and is completely dependent on his family for his activities of daily living. He has a loud P2, an ejection systolic murmur over the tricuspid region and a right ventricular heave. His JVP is elevated without ‘a’ waves but prominent ‘v’ waves. He has shifting dullness and peripheral oedema up to mid thigh. His ECG shows signs of right ventricular hypertrophy, and his ECHO estimates a systolic pulmonary pressure of 55mmHg using the estimated tricuspid jet velocity in ‘M’ mode.
What chest X-ray imaging sign would be LEAST associated with pulmonary hypertension
(A) Cardiomegaly
(B) Pulmonary Arterial Pruning
(C) Right Upper Lobe consolidation with air-bronchograms
(D) Bi-basal predominant interstitial infiltrates resembling fibrosis
(E) Hampton’s hump
Question 7: Clinical Diagnosis
A 28 year-old man is suspected of having idiopathic pulmonary artery hypertension with a JVP measuring 5cm above sternal notch. He has an echocardiogram performed. The views were of sufficient quality, enabling the sonographer to calculate the following parameters:
Tricuspid regurgitant jet velocity: 4m.s-1
Left ventricular Ejection Fraction using Simpsons Method: 58%
Fractional shortening: 37%
What is the BEST fit for calculated parameters of Pressure gradient (dP), Right atrial Pressure, Systolic Pressure and Diagnosis
Answer
(A) Pressure gradient (dP) 64, RAP 10, sPAP 54, Diagnosis: Pulmonary hypertension
(B) Pressure gradient (dP)64, RAP 10, sPAP 74, Diagnosis: Undetermined
(C) Pressure gradient (dP) 64, RAP 5, sPAP 69, Diagnosis: Undetermined
(D) Pressure gradient (dP) 48, RAP 5, sPAP 53, Diagnosis: Pulmonary Hypertension
(E) Pressure gradient (dP) 48, RAP 10, sPAP 58, Diagnosis: Pulmonary Hypertension
Question 9: Categories of pulmonary hypertension
Once the diagnosis of pulmonary arterial hypertension is distinguished from pulmonary venous hypertension, which of the below options does NOT adequately help distinguish a cause
(A) ANA and interstitial lung disease
(B) V/Q and CTPEH
(C) anti-scl70 and diffuse scleroderma
(D) anti-centromere and limited scleroderma
(E) HIV third generation antigen/ antibody and HIV
Question 10: Causes
Which of the following medications are NOT associated with idiopathic pulmonary arterial hypertension
(A) dasatinib
(B) appetite suppressants
(C) St Johns wort
(D) chronic cocaine use
(E) obinutuzumab
Question 11: Treatment
A 68 year-old male with idiopathic pulmonary hypertension is undergoing consideration for treatment. Which of the following statements is FALSE about the role of anti-coagulation.
(A) Warfarin is the anticoagulation of choice because other studies are lacking
(B) A meta-analysis of seven observational studies has shown a benefit favouring anti-coagulation in terms of mortality
(C) There is no difference in bleeding risk in patients with PAH secondary to connective tissue disease in comparison to patients with idiopathic pulmonary hypertension
(D) There is no evidence for use of anticoagulation in PAH due to anorexigens
(E) The rationale for anti-coagulation is due to sluggish pulmonary blood flow leading to a predisposition for thrombosis on the background of poor physiological reserve
Question 12: Treatment
Which patient group is most likely to respond to the nitrous oxide vasoreactivity test?
(A) Pulmonary arterial hypertension secondary to non-specific interstitial pneumonia
(B) Pulmonary arterial hypertension secondary to drugs such as anorexigen
(C) Pulmonary arterial hypertension secondary to HIV
(D) Pulmonary arterial hypertension secondary to schistosomiasis
(E) Pulmonary arterial hypertension secondary to PTPN22a mutation
Question 13: Treatment
What is the mortality of a patient who has pulmonary arterial hypertension who falls pregnant?
(A) 17 – 33%
(B) 2 – 12%
(C) 35 – 60%
(D) 50 – 70%
(E) 60 – 85%
Question 14: Treatment
Which of the following statements is INCORRECT
(A) Bosentan and ambrisentan are endothelin receptor antagonists, functionally causing a pulmonary vasodilated state, with Bosentan causing reversible liver function abnormalities in 10% requiring monthly LFT monitoring
(B) Sildanefil and tadalafil inhibit phosphodiesterase 5, which causes increased cyclic GMP via nitrous oxide therefore causing pulmonary smooth muscle vasodilation. Its use is contra-indicated with other nitrates
(C) One criterion of the PBS states that right heart catheterisation should be used and the criterion is that the mean pulmonary arterial pressure is greater than 25 mmHg with the pulmonary capillary wedge pressure less than 15mmHg
(D) Prostanoids are prostacyclins that cause pulmonary arterial vasodilation with added anti-proliferative effects
(E) Riociguat cannot be used for the treatment of pulmonary artery hypertension secondary to chronic thromboembolic disease
