Question 1
What is TRUE regarding the risks of hormone replacement therapy as according to the women's health initiative study?
(A) It increases the risk of stroke in women under the age of 60
(B) It doubles the risk of deep vein thrombosis
(C) It increases the risk of colorectal cancer
(D) There is one extra case of breast cancer per 100 patients on HRT, per annum
(E) It increases the risk of ovarian cancer
B: The risk of stroke is increased in women over the age of 60. Data suggest that the timing of treatment initiation affects the risk of CHD; in the WHI, women who were <10 years since menopause or between the ages of 50 to 59 years did not have excess risk. In the Women’s Health Initiative (WHI), the risk of invasive breast cancer was significantly increased with combined hormone therapy (HT) at an average follow-up of 5.6 years. There is approximately one extra case of breast cancer per 1000 patients on HRT per annum. There is a non significant increase in ovarian cancer risk, but this is controversial. Colorectal cancer risk is reduced. Ann Intern Med 2013; 158:47.
Question 2
What is TRUE regarding periprocedural myocardial infarctions?
(A) They are rare events
(B) They typically occur in the first 48 hours post procedure when analgesia may mask symptoms of chest pain
(C) Randomised Control Trials of periprocedural myocardial infarctions show no benefit for commonly used secondary prevention drugs
(D) Pre-operative troponin levels do not predict poor outcome post procedure
(E) Pre-operative aspirin decreases myocardial infarction rates perioperatively at the expense of an increased risk of major bleeding
B: 65% of patients do not have symptoms of myocardial ischaemia in the perioperative period. Most myocardial infarctions also happen in the first 48 hours for this reason, and some experts have advocated that post-operative troponins be used in order to potentially detect these patients. N Engl J Med 2015; 373:2258-2269
Question 3
A 64 year old female with hypertension and type 2 diabetes who is currently on aspirin attends the perioperative medicine clinic for assessment prior to elective hip replacement. The anaesthetist gives the patient advice on blunting the sypmathetic stress response with the use of either clonidine or beta-blockers. What is the correct response?
(A) Beta blockers used for the purpose of the perioperative period sympathetic response inhibition decreases non fatal myocardial infarctions at the risk of death, non fatal stroke and bradycardia
(B) Clonidine decreases myocardial infarction rates
(C) Clonidine increases the rates of non fatal strokes when used in the periprocedural setting
(D) Beta-blockers should be discontinued in all patients
(E) Clonidine increases the risk of aspiration pneumonia
A: N Engl J Med 2015; 373:2258-2269
Question 4
What is the strongest prognostic biomarker for death or myocardial infarction in the perioperative setting?
(A) high sensitivity troponin
(B) NT-pro-BNP
(C) high sensitivity CRP
(D) CK-MZB
(E) muscle specific aldolase
B: "In a meta-analysis of individual data from 2179 patients, of whom 235 died or had a myocardial infarction (the primary outcome) within 30 days after noncardiac surgery, an elevated preoperative plasma level of natriuretic peptide (i.e., a B-type natriuretic peptide [BNP] level of ≥92 ng per liter or an N-terminal pro-BNP [NT-proBNP] level of ≥300 ng per liter) was the strongest independent preoperative predictor of the primary outcome (odds ratio, 3.40; 95% CI, 2.57 to 4.47)" N Engl J Med 2015; 373:2258-2269
Question 5
What is the recommended time that vitamin K antagonists should be ceased prior to invasive surgery?
(A) 1 days
(B) 3 days
(C) 5 days
(D) 7 days
(E) 10 days
C: guideline suggests stopping warfarin five days before the procedure and restarting it 12-24 hours afterwards, assuming that adequate hemostasis is maintained. BMJ 2015;351:h2391
Question 6
A 64 year old male is undergoing a TURP procedure for refractory benign prostatic hyperplasia. He also has atrial fibrillation for which he is on dabigatran. His estimated creatinine clearance is 42 ml/ min. He has previously had minor bleeding events after skin surgery. What is the recommended time prior to the procedure that dabigatran should be witheld?
(A) 12 h
(B) 24 h
(C) 48 h
(D) 72 h
(E) 96 h
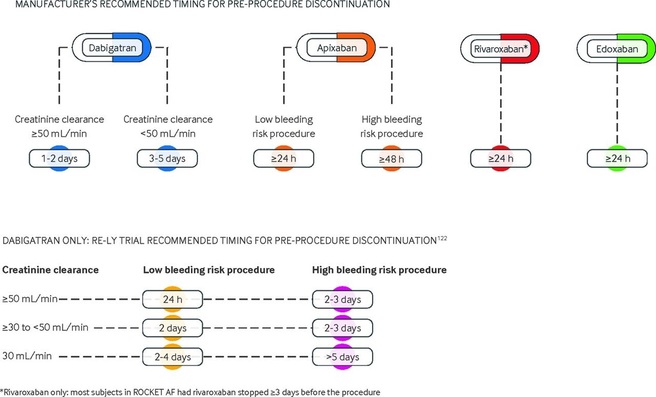
D: For high risk bleeding procedures (such as TURP), in patients with a CrCl 30 - 50 ml/min, the recommended pre-procedure cessation interval is 2 - 3 days. If the creatinine clearance is <30, then I would stop >= 5d. BMJ 2015;351:h2391 (see below for picture courtesy of BMJ)
What is TRUE regarding the risks of hormone replacement therapy as according to the women's health initiative study?
(A) It increases the risk of stroke in women under the age of 60
(B) It doubles the risk of deep vein thrombosis
(C) It increases the risk of colorectal cancer
(D) There is one extra case of breast cancer per 100 patients on HRT, per annum
(E) It increases the risk of ovarian cancer
B: The risk of stroke is increased in women over the age of 60. Data suggest that the timing of treatment initiation affects the risk of CHD; in the WHI, women who were <10 years since menopause or between the ages of 50 to 59 years did not have excess risk. In the Women’s Health Initiative (WHI), the risk of invasive breast cancer was significantly increased with combined hormone therapy (HT) at an average follow-up of 5.6 years. There is approximately one extra case of breast cancer per 1000 patients on HRT per annum. There is a non significant increase in ovarian cancer risk, but this is controversial. Colorectal cancer risk is reduced. Ann Intern Med 2013; 158:47.
Question 2
What is TRUE regarding periprocedural myocardial infarctions?
(A) They are rare events
(B) They typically occur in the first 48 hours post procedure when analgesia may mask symptoms of chest pain
(C) Randomised Control Trials of periprocedural myocardial infarctions show no benefit for commonly used secondary prevention drugs
(D) Pre-operative troponin levels do not predict poor outcome post procedure
(E) Pre-operative aspirin decreases myocardial infarction rates perioperatively at the expense of an increased risk of major bleeding
B: 65% of patients do not have symptoms of myocardial ischaemia in the perioperative period. Most myocardial infarctions also happen in the first 48 hours for this reason, and some experts have advocated that post-operative troponins be used in order to potentially detect these patients. N Engl J Med 2015; 373:2258-2269
Question 3
A 64 year old female with hypertension and type 2 diabetes who is currently on aspirin attends the perioperative medicine clinic for assessment prior to elective hip replacement. The anaesthetist gives the patient advice on blunting the sypmathetic stress response with the use of either clonidine or beta-blockers. What is the correct response?
(A) Beta blockers used for the purpose of the perioperative period sympathetic response inhibition decreases non fatal myocardial infarctions at the risk of death, non fatal stroke and bradycardia
(B) Clonidine decreases myocardial infarction rates
(C) Clonidine increases the rates of non fatal strokes when used in the periprocedural setting
(D) Beta-blockers should be discontinued in all patients
(E) Clonidine increases the risk of aspiration pneumonia
A: N Engl J Med 2015; 373:2258-2269
Question 4
What is the strongest prognostic biomarker for death or myocardial infarction in the perioperative setting?
(A) high sensitivity troponin
(B) NT-pro-BNP
(C) high sensitivity CRP
(D) CK-MZB
(E) muscle specific aldolase
B: "In a meta-analysis of individual data from 2179 patients, of whom 235 died or had a myocardial infarction (the primary outcome) within 30 days after noncardiac surgery, an elevated preoperative plasma level of natriuretic peptide (i.e., a B-type natriuretic peptide [BNP] level of ≥92 ng per liter or an N-terminal pro-BNP [NT-proBNP] level of ≥300 ng per liter) was the strongest independent preoperative predictor of the primary outcome (odds ratio, 3.40; 95% CI, 2.57 to 4.47)" N Engl J Med 2015; 373:2258-2269
Question 5
What is the recommended time that vitamin K antagonists should be ceased prior to invasive surgery?
(A) 1 days
(B) 3 days
(C) 5 days
(D) 7 days
(E) 10 days
C: guideline suggests stopping warfarin five days before the procedure and restarting it 12-24 hours afterwards, assuming that adequate hemostasis is maintained. BMJ 2015;351:h2391
Question 6
A 64 year old male is undergoing a TURP procedure for refractory benign prostatic hyperplasia. He also has atrial fibrillation for which he is on dabigatran. His estimated creatinine clearance is 42 ml/ min. He has previously had minor bleeding events after skin surgery. What is the recommended time prior to the procedure that dabigatran should be witheld?
(A) 12 h
(B) 24 h
(C) 48 h
(D) 72 h
(E) 96 h
D: For high risk bleeding procedures (such as TURP), in patients with a CrCl 30 - 50 ml/min, the recommended pre-procedure cessation interval is 2 - 3 days. If the creatinine clearance is <30, then I would stop >= 5d. BMJ 2015;351:h2391 (see below for picture courtesy of BMJ)
Question 7
A 64 year old male presents with haemetemesis and malena. He is normotensive, tachycardic and immediate fluid resuscitation is instituted. Medications include aspirin and dabigatran. His thrombin time is within normal range, as are his other coagulation studies. His Hb is 64. Platelets are normal. With regards to blood product management, what is the best strategy?
(A) Activated factor 7
(B) Platelets and packed blood
(C) Platelets, packed blood and prothrombin complex
(D) cryoprecipitate
(E) Platelets, packed blood and fresh frozen plasma
B: There is no significant dabigatran effect as the thrombin time is normal. However, the effects of aspirin on platelets should be countered by platelet transfusion. Cryoprecipitate is enriched in fibrinogen and factor VIII.
Question 8
What is most likely to be found on a skin biopsy of psoriasis?
(A) Neutrophillic infiltrate
(B) Lymphocytic infiltrate
(C) Epidermis desquamation
(D) Dermal desquamation
(E) Submucosal angiogenesis
A: PEP lecture 2014
Question 9
Which of the following is a known cause of raised anion gap metabolic acidosis without raised lactate or ketones?
(A) pyroglutamic acidosis
(B) renal tubular acidosis
(C) Frusemide abuse
(D) Excessive diarrhoea
(E) Barter’s syndrome
A: Pyroglutamic acidosis is a rare cause of acidosis that has been described. It is a raised anion gap metabolic acidosis occurring in the context of normal lactate, ketones, normal osmolar gap and no evidence of toxic alcohol metabolites. It may be diagnosed by determination of organic acids in urine. Pyroglutamic acid is synthesised by GGT, which is increased in the setting of decreased glutathione stores. Case studies have showed this type of acidosis to occur in patients with sepsis, use of flucloxacillin (where 5-oxyprolinase is inhibited, which is the catabolic enzyme that degrades pyroglutamic acid) and in other states of decreased glutathione.
Question 10
Non-anion gap metabolic acidosis results from all of the following conditions except?
(A) Diarrhoea
(B) Vomiting
(C) ileal conduit
(D) Renal tubular acidosis
(E) carbonic anhydrase inhibitors
B: Vomiting causes a metabolic alkalosis through the expulsion of H+ in stomach acid, and the subsequent production of HCO3 in order to compensate for further production of H+ in the gastric parietal cells.
Question 11
A 32-week old pregnant lady has a motor vehicle accident and suffers from a fractured fibula and bruises to her chest. Fortunately her abdomen is not injured and her fetus remains in good health. She is treated with regular analgesia with good effect. The nurse alerts the medical officer due to decreased level of consciousness. An arterial blood gas is performed which reveals the following variables: pH 7.30, CO2 42, HCO3 21, BE -6, lactate 0.5, Anion gap 8. Which of the following best describes her acid base balance?
(A) Primary respiratory acidosis
(B) Mixed respiratory and metabolic acidosis
(C) Respiratory acidosis and metabolic alkalosis
(D) Normal acid base status
(E) Metabolic acidosis with respiratory alkalosis
A: Normally due to pregnancy related changes in respiratory physiology, the pCO2 is maintained at 30mmHg, with a subsequent compensatory HCO3 loss. Whilst this appears to be a combined respiratory and metabolic acidosis on face value, one must take pregnancy related physiological changes to account. The respiratory acidosis is explained by the effects of narcotic analgesia on the respiratory centre.
Question 12
Which of the following describes the correct association between anion gap and measured variables?
(A) Decrease in albumin decreases the anion gap
(B) Increased bicarbonate increases the anion gap
(C) Increased Chloride increases the anion gap
(D) Decreased calcium decreases the anion gap
(E) Decreased Sodium increases the anion gap
A: The anion gap is a derived variable, mathematically calculated as Na – [ HCO3 + Cl-]. The greatest proportion of the anion gap represents serum albumin, which carries a negative charge.
Question 13
A 42-year old patient is on continuous veno-venous hemodiafiltration in ICU and is ventilated, after suffering from sepsis related acute kidney injury and ARDS. An arterial blood gas reveals a normal anion gap metabolic alkalosis, with decreased serum albumin and lactate 7. What is the most likely correct interpretation?
(A) Metabolic alkalosis is secondary to frusemide therapy
(B) Metabolic alkalosis is related to conversion of lactate to bicarbonate from the diasylate fluid. However the excess lactate is unable to be converted to bicarbonate, leading to a lactataemia. The anion gap is normal because of elevated bicarbonate and decreased serum albumin
(C) Metabolic alkalosis related to permissive hypercapnia as a form of lung protection ventilation in ARDS. Hyperlactatemia secondary to poor tissue microperfusion related to sepsis.
(D) Normal anion gap metabolic alkalosis as a result of increased nasogastric aspirates
(E) Metabolic alkalosis relating to administration of sodium bicarbonate in order to compensate for hyperlactatemia.
B
A 64 year old male presents with haemetemesis and malena. He is normotensive, tachycardic and immediate fluid resuscitation is instituted. Medications include aspirin and dabigatran. His thrombin time is within normal range, as are his other coagulation studies. His Hb is 64. Platelets are normal. With regards to blood product management, what is the best strategy?
(A) Activated factor 7
(B) Platelets and packed blood
(C) Platelets, packed blood and prothrombin complex
(D) cryoprecipitate
(E) Platelets, packed blood and fresh frozen plasma
B: There is no significant dabigatran effect as the thrombin time is normal. However, the effects of aspirin on platelets should be countered by platelet transfusion. Cryoprecipitate is enriched in fibrinogen and factor VIII.
Question 8
What is most likely to be found on a skin biopsy of psoriasis?
(A) Neutrophillic infiltrate
(B) Lymphocytic infiltrate
(C) Epidermis desquamation
(D) Dermal desquamation
(E) Submucosal angiogenesis
A: PEP lecture 2014
Question 9
Which of the following is a known cause of raised anion gap metabolic acidosis without raised lactate or ketones?
(A) pyroglutamic acidosis
(B) renal tubular acidosis
(C) Frusemide abuse
(D) Excessive diarrhoea
(E) Barter’s syndrome
A: Pyroglutamic acidosis is a rare cause of acidosis that has been described. It is a raised anion gap metabolic acidosis occurring in the context of normal lactate, ketones, normal osmolar gap and no evidence of toxic alcohol metabolites. It may be diagnosed by determination of organic acids in urine. Pyroglutamic acid is synthesised by GGT, which is increased in the setting of decreased glutathione stores. Case studies have showed this type of acidosis to occur in patients with sepsis, use of flucloxacillin (where 5-oxyprolinase is inhibited, which is the catabolic enzyme that degrades pyroglutamic acid) and in other states of decreased glutathione.
Question 10
Non-anion gap metabolic acidosis results from all of the following conditions except?
(A) Diarrhoea
(B) Vomiting
(C) ileal conduit
(D) Renal tubular acidosis
(E) carbonic anhydrase inhibitors
B: Vomiting causes a metabolic alkalosis through the expulsion of H+ in stomach acid, and the subsequent production of HCO3 in order to compensate for further production of H+ in the gastric parietal cells.
Question 11
A 32-week old pregnant lady has a motor vehicle accident and suffers from a fractured fibula and bruises to her chest. Fortunately her abdomen is not injured and her fetus remains in good health. She is treated with regular analgesia with good effect. The nurse alerts the medical officer due to decreased level of consciousness. An arterial blood gas is performed which reveals the following variables: pH 7.30, CO2 42, HCO3 21, BE -6, lactate 0.5, Anion gap 8. Which of the following best describes her acid base balance?
(A) Primary respiratory acidosis
(B) Mixed respiratory and metabolic acidosis
(C) Respiratory acidosis and metabolic alkalosis
(D) Normal acid base status
(E) Metabolic acidosis with respiratory alkalosis
A: Normally due to pregnancy related changes in respiratory physiology, the pCO2 is maintained at 30mmHg, with a subsequent compensatory HCO3 loss. Whilst this appears to be a combined respiratory and metabolic acidosis on face value, one must take pregnancy related physiological changes to account. The respiratory acidosis is explained by the effects of narcotic analgesia on the respiratory centre.
Question 12
Which of the following describes the correct association between anion gap and measured variables?
(A) Decrease in albumin decreases the anion gap
(B) Increased bicarbonate increases the anion gap
(C) Increased Chloride increases the anion gap
(D) Decreased calcium decreases the anion gap
(E) Decreased Sodium increases the anion gap
A: The anion gap is a derived variable, mathematically calculated as Na – [ HCO3 + Cl-]. The greatest proportion of the anion gap represents serum albumin, which carries a negative charge.
Question 13
A 42-year old patient is on continuous veno-venous hemodiafiltration in ICU and is ventilated, after suffering from sepsis related acute kidney injury and ARDS. An arterial blood gas reveals a normal anion gap metabolic alkalosis, with decreased serum albumin and lactate 7. What is the most likely correct interpretation?
(A) Metabolic alkalosis is secondary to frusemide therapy
(B) Metabolic alkalosis is related to conversion of lactate to bicarbonate from the diasylate fluid. However the excess lactate is unable to be converted to bicarbonate, leading to a lactataemia. The anion gap is normal because of elevated bicarbonate and decreased serum albumin
(C) Metabolic alkalosis related to permissive hypercapnia as a form of lung protection ventilation in ARDS. Hyperlactatemia secondary to poor tissue microperfusion related to sepsis.
(D) Normal anion gap metabolic alkalosis as a result of increased nasogastric aspirates
(E) Metabolic alkalosis relating to administration of sodium bicarbonate in order to compensate for hyperlactatemia.
B