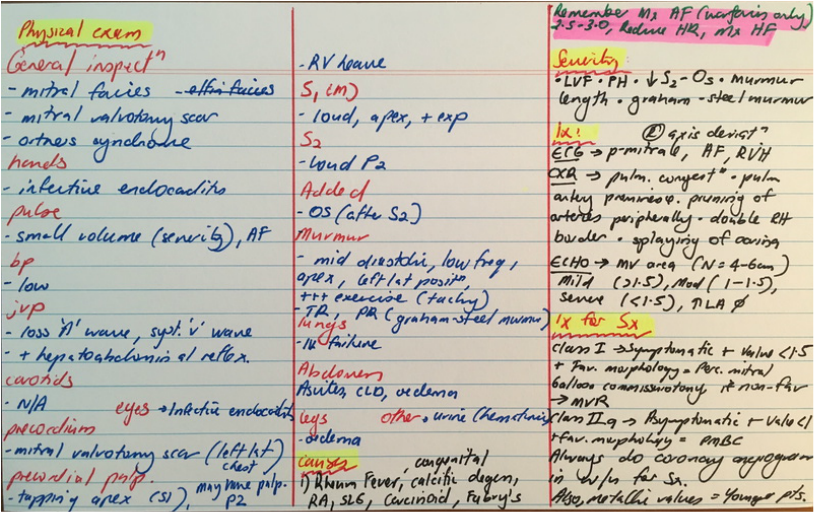
Mitral Stenosis
Explain the cause of the first heart sound?
What are the causes of a loud first heart sound?
What are the causes of a soft first heart sound
Describe the finding of the opening snap in a patient with mitral stenosis
What is the reason behind the inverse correlation of severity of mitral stenosis and the length of S2-OS
What is an important differential for MS?
What is the medical management of MS?
What are the surgical options for treating MS?
- It corresponds to the closure of the atrioventricular valves. The exact cause is debated, but is thought to occur due to abrupt cessation of moving blood columns secondary to the closure of the valves, and the rapid deceleration which causes the chordae tendinae, papillary muscles and ventricles to vibrate
- The intensity of S1 is due to the force of ventricular contraction and also the position of the atrioventricular valves at the onset of ventricular systole
What are the causes of a loud first heart sound?
- Due to rapid ventricular contraction, as occurs with fever and other sympathetic stimulation such as SABA, thyrotoxicosis
- Delayed closure of the AV valves. After atrial systole and when the ventricles begin to contract, the AV valves are held wider apart, therefore it takes longer for them to close, and when they do finally oppose each other to close, they shut at a rapid rate of deceleration because the ventricle has had enough time to generate a vigorous contraction
- Prolapsed mitral valve because the mitral valves that prolapse take longer to tense up and thus close at a time when ventricular contraction is more forceful
- Mitral stenosis because the pressure gradient of the LA - LV keeps the valves apart for longer and hence they take longer to close
- Short PR interval: Ventricular systole occurs shortly after atrial systole.
- Atrial myxoma: the tumour falls into the mitral orifice and hence there is delayed closure of the valve
What are the causes of a soft first heart sound
- Poor ventricular contraction due to cardiomyopathy
- LBBB
- Prolonged PR interval: The atrial systole has occured and the atria is relaxing whilst the ventricle is filling, and when ventricular systole occurs, the mitral valve is more closely apposed. Therefore there is not enough time for the contraction to build up in strength to cause a forceful closure of the valve
- Acute aortic regurgitation: The regurgitant volume fills the ventricle in diastole. When it is acute (ie infective endocarditis) there is not enough time for the ventricle to remodel itself in order to become more compliant. Subsequently the LV diastolic pressures increase and may match LA pressures, causing opposition of the mitral valve leaflets
Describe the finding of the opening snap in a patient with mitral stenosis
- The opening snap occurs just prior to the diastolic rumbling murmur of mitral stenosis
- The mechanism is thought to relate to the mitral valve billowing out into the LV due to the pressure gradient created by the stenosis, and as the maximum angles of movement are reached, the leaflets of the mitral valve rapidly decelerate creating the sound.
- It is heard best at the apex, or between the apex and the left lower sternal border
What is the reason behind the inverse correlation of severity of mitral stenosis and the length of S2-OS
- The tighter the stenosis the greater is the atrial force required to overcome the stenosis
- Therefore the mitral valve opens earlier in diastole
What is an important differential for MS?
- left atrial myxoma, which in stead of an opening snap causes a tumour plop
- This may be seen in TTE
What is the medical management of MS?
- Medical therapy does not alter natural history of lesion and does not delay surgery
- Medical treatment is directed toward alleviating pulmonary congestion with diuretics, treating atrial fibrillation, and anti-coagulating patients who are at increased risk of arterial embolic events.
- Tachycardia is typically poorly tolerated in patients with MS and can lead to an acute deterioration as diastolic filling time may be inadequate. In particular, heart rate control can be beneficial in patients with MS and atrial fibrillation and fast ventricular response
- However, heart rate control may also be considered for patients with MS in normal sinus rhythm and symptoms associated with exercise
- Anticoagulation with warfarin is indicated to prevent thromboembolism when atrial fibrillation is present, if there is a prior history of thromboembolism, or if a thrombus is detected in the left atrium.
- Anticoagulation may also be considered if the left atrium is markedly dilated (5.0-5.5 mm) or if there is spontaneous contrast on echocardiography (Class IIb).
- Long-term secondary prophylaxis is recommended for all patients with a history of rheumatic fever, rheumatic carditis or rheumatic valve disease because recurrent carditis can occur at a higher frequency after previous carditis and this can cause acceleration of the lesions natural history.
What are the surgical options for treating MS?
- percutaneous mitral balloon commissurotomy
- catheter-based technique in which a balloon is inflated across the stenotic valve to split the fused commissures and increase the valve area
- comparable with those achieved with open mitral commissurotomy
- need favourable valve morphology - Severe valve calcification and/or significant thickening/calcification of the subvalvular apparatus on echocardiography before PMBC is associated with a higher complication rate and a greater risk of recurrence.
- not to be done if there is LA thrombus or there is MR
- Class 1/ II indications:
- severe symptomatic MS (<1.5cm sq valve area)
- less severe symptomatic MS (valve area > 1.5cm sq) but haemodynamically significant MS on exercise
- asymptomatic MS (<1cm sq valve area)
- severe symptomatic MS (<1.5cm sq valve area)
- catheter-based technique in which a balloon is inflated across the stenotic valve to split the fused commissures and increase the valve area
- open mitral commissurotomy
- Surgical mitral commissurotomy (either open or closed) may be carried out through a median sternotomy or left thoracotomy incision
- Surgical mitral commissurotomy (either open or closed) may be carried out through a median sternotomy or left thoracotomy incision
- mitral valve replacement
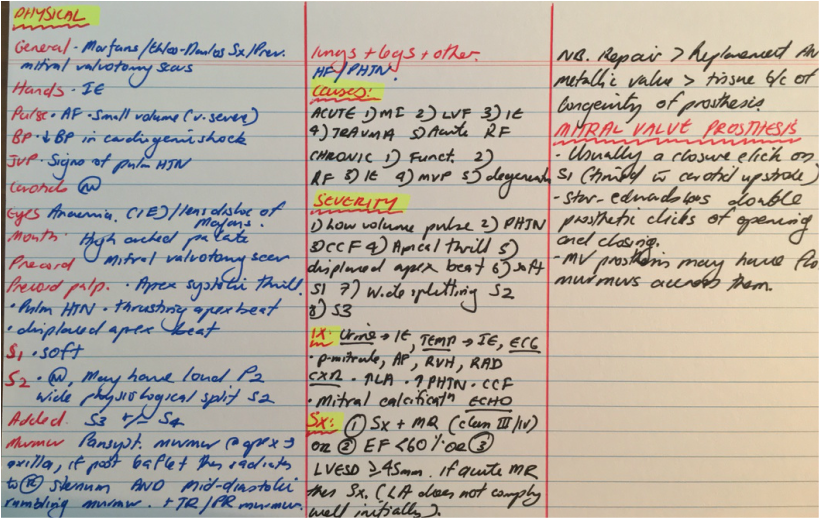
Mitral Regurgitation
- Mostly, the murmur is pansystolic, loudest at apex, radiating to the axilla
- In some patients who have isolated incompetence of the medial portion of the posterior leaflet, the murmur radiates to the right base and perhaps into the neck, therefore mimicking AS
Severity of secondary MR
- effective regurgitant orifice area (EROA) is ≥0.2 cm2
- regurgitant volume is ≥30cc
- if the patient is symptomatic (Stage D)
Severity of primary MR
- LVESD ≥40 mm
- left ventricular ejection fraction ≤60%
- EROA ≥0.4 cm2
Management of acute severe MR
- Medical emergency because the LV has not had time to dilate to cope with the volume overload from the regurgitation
- LA and pulmonary pressures build, causing acute pulmonary oedema
- Reduce afterload with SNP or GTN infusion
- IABP may stabilise these patients
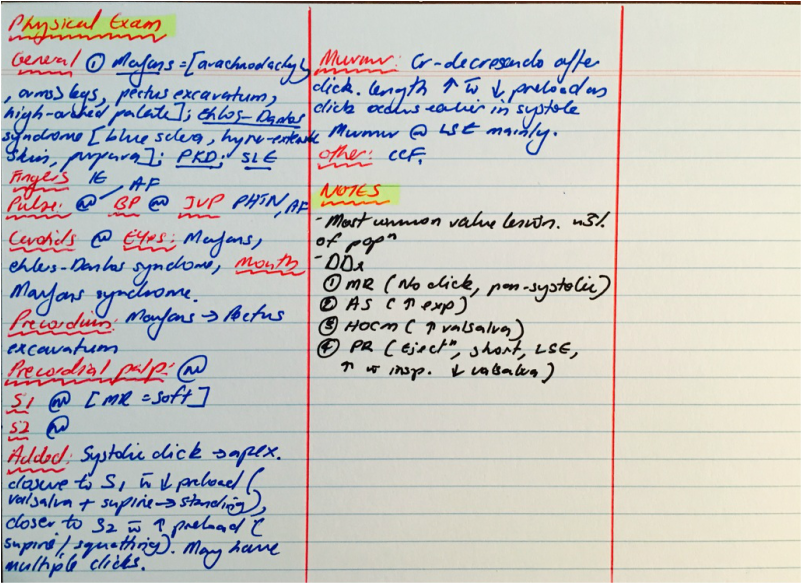
Mitral Valve Prolapse
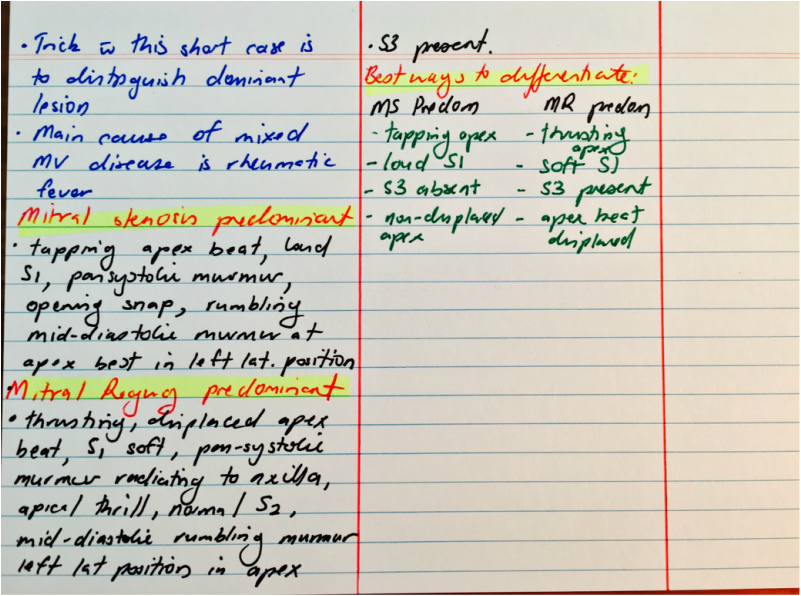
Mixed Mitral Disease
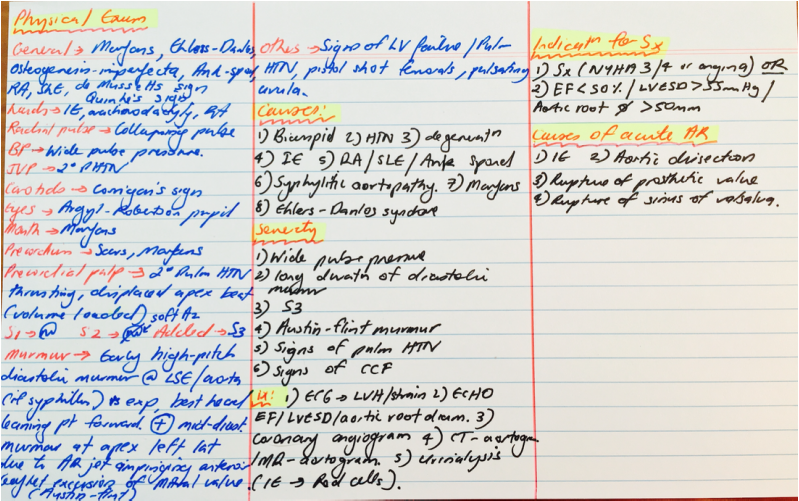
Aortic Regurgitation
What are the three murmurs that may be audible with aortic regurgitation?
What is the mechanism behind the water-hammer pulse of acute aortic regurgitation?
What is the significance of the early diastolic decrescendo murmur of aortic regurgitation being heard at the right sternal edge?
What does inhalation of amyl nitrate do to the diastolic murmur of aortic regurgitation?
What is the pulse pressure difference that is required for aortic regurgitation to be considered in the differential diagnosis?
- Early decrescendo diastolic murmur which is blowing and high frequency, loudest at the LSE 3rd or 4th interspace. It may only be audible with the patient sitting forward with their breath held in expiration
- Systolic flow murmur through the aortic valve
- Austin flint murmur
What is the mechanism behind the water-hammer pulse of acute aortic regurgitation?
- The sudden rise and rapid fall of occurs because there is a large regurgitant volume followed by aortic run-off. This is exagerated when the examiner raises the arm such that the diastolic pressure in the radial artery decreases, and hence the collapsing nature is accentuated.
- Furthermore systolic pulse is accentuated because by raising the arm there is more regurgitant run-off secondary to increased gravitational effect.
What is the significance of the early diastolic decrescendo murmur of aortic regurgitation being heard at the right sternal edge?
- Its presence increases the likelihood ratio of the presence of aortic root disease, such as marfan syndrome, aortic dissection, syphilitic aortitis or damage to a single aortic cusp.
- It is thought to be caused by an eccentric regurgitant jet
What does inhalation of amyl nitrate do to the diastolic murmur of aortic regurgitation?
- Amyl nitrate is a vasodilator and decreases diastolic pressures
- Therefore there is a decreased pressure gradient between the aorta and left ventricle during diastole
- This test was helpful in distinguishing between pulmonary regurgitation (graham-steel murmur) and aortic regurgitation, especially if there was no change with the respiratory cycle.
What is the pulse pressure difference that is required for aortic regurgitation to be considered in the differential diagnosis?
- >80mmHg (LR 10.9)
- Diastolic blood pressure 50mmHg or less (LR 19.3)
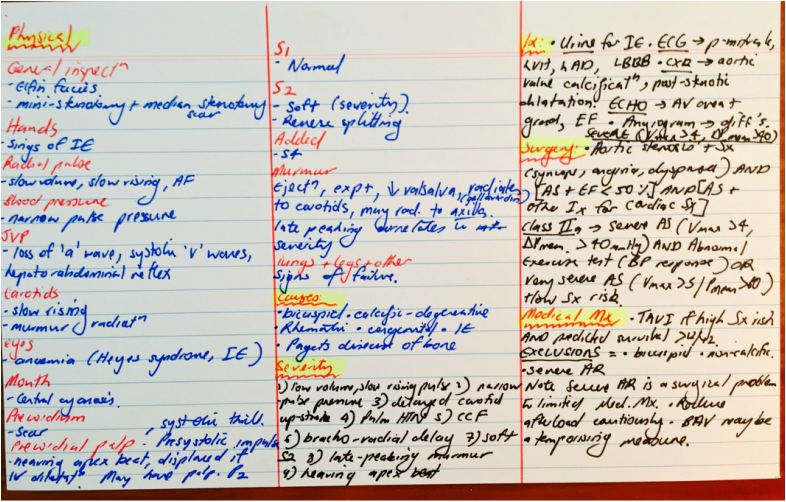
Aortic Stenosis
What is the gallavardin's phenomenon?
Why do patients with aortic stenosis have a bleeding tendency?
- A musical-quality, holosytolic murmur is present at the apex of the heart that occurs in older patients with calcific AS, which may mimic mitral regurgitation.
Why do patients with aortic stenosis have a bleeding tendency?
- Patients have an increased risk of bleeding and may complain of epistaxis or bruising. They are also more likely to develop chronic gastrointestinal bleeding that is associated with angiodysplasia.
- Turbulent flow across the stenotic valve may produce an acquired von Willebrand deficiency.
- The prevalence of bleeding is 20%.
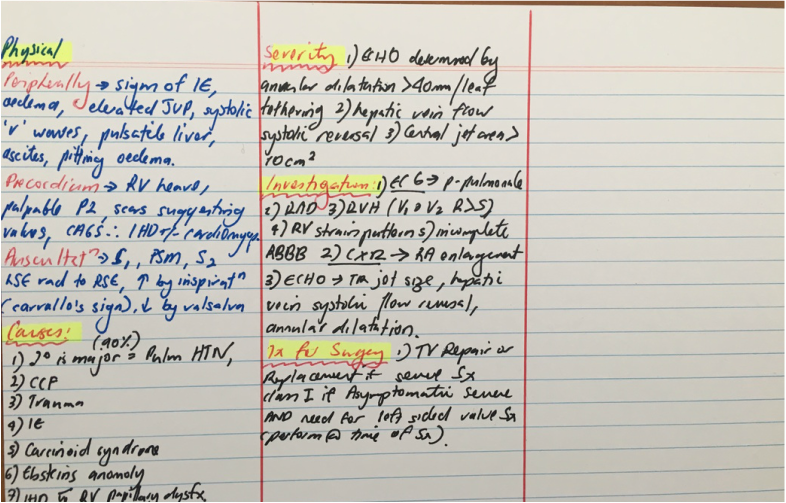
Tricuspid Regurgitation
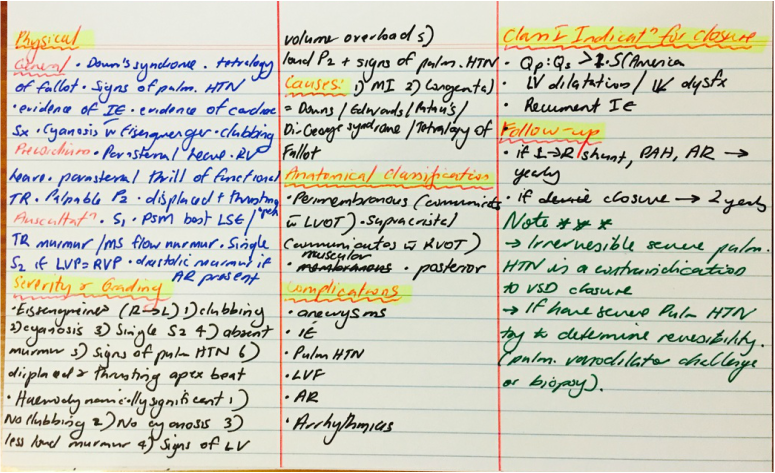
Ventricular Septal Defect
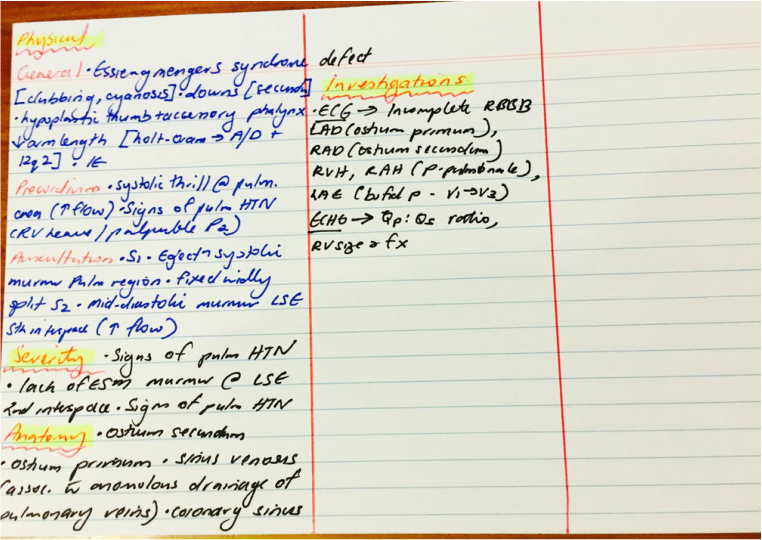
Atrial Septal Defect
Hypertrophic Obstructive Cardiomyopathy
General inspection
- Not much to report
- Infective endocarditis is a recognised complication of HOCM
- Pulse AF
- May have pulsus bisferiens - double peak per cardiac cycle is appreciated
- BP may be low
- Loss of 'a' waves if in AF
- Because of marked septal hypertrophy there may be very prominent 'a' waves
- Prominent carotid pulsation with a double carotid arterial impulse
- Presystolic accentuation (not if there is loss of atrial contraction in AF) resulting in a double apical impulse
- Heaving apex beat
- Parasternal heave due to turbulent flow in the LV outflow tract
- Apical thrill if there is MR with systolic anterior motion of the mitral valve
- S1 is normal
- S2 has reversed splitting
- S4 due to atrial contraction against a non compliant LV
- Crescendo-decrescendo murmur in HOCM heard best at LSE, radiating up the sternal border but not to the carotids
- Increased intensity of murmur with valsalva and standing from squatting position
How would you investigate this patient?
- ECG showing evidence of LVH on voltage criterion, LVH strain pattern, LAD, L atrial dilatation, dagger q waves in leads II, III and aVF or V2 - V6, AF
- The apical form of HCM (Yamaguchi's disease) may show deep T-wave inversions across the antero-apical leads.
- CXR: Cardiomegaly, LAD as evidenced by a double right heart border or prominent left atrial appendage
- ECHO: LVH, asymmetric septal hypertrophy, systolic anterior motion of the mitral valve, diastolic dysfunction
- Cardiac MRI
- Catheter studies: A classic finding in HCM is the Brockenbrough-Braunwald-Morrow sign, in which the left ventricle-to-aortic gradient increases while the aortic pulse pressure decreases following premature ventricular contraction (PVC). Such a phenomenon occurs in HCM due to increased contractility in the post-PVC beat, which can cause an increase in the dynamic LVOT obstruction.
What is the most common genetic mutation found in hypertrophic obstructive cardiomyopathy?
- 35 diff genes with 100s of mutations with marked phenotypic heterogeneity.
- Most important = beta-myosin heavy chain and myosin binding protein C
What is the reason that the valsalva manoeuvre increases the intensity of the HOCM left sternal edge ejection systolic murmur?
- During the straining phase of the valsalva manouvre, there is increased intrathoracic pressure and therefore decreased venous return
- As a consequence, the mitral anterior leaflet and the septum are brought closer together and therefore aggravates the obstruction
- increased return moves the mitral leaflet and the septal wall further apart
- Squatting to standing manouvre also increases the intensity of the HOCM manoeuvre, whilst standing to squatting decreases the intensity, as does passive leg elevation (increasing venous return)
What are the two manoeuvres that increase the intensity of the murmur of mitral regurgitation and VSD
- Isometric hand grip and transient arterial occlusion causes increased afterload.
- In MR and VSD, because there are two pathways of exit from blood flow out of the ventricular cavity, the intensity of the murmur increases
Why are vasodilators contra-indicated in left ventricular outflow obstruction?
- By decreasing the afterload through vasodilation, the left ventricular fractional shortening is shorter in time, and therefore this augments the dynamic obstruction that occurs due to the septal hypertrophy
What is the reason for the double carotid impulse and pulsus bisferiens?
- With HCM, the carotid upstroke is brisk, because there is little resistance during early systole in ejecting the blood through the LVOT into the aorta.
- As systole progresses, and blood flow is ejected, the anterior leaflet of the mitral valve and the hypertrophied septum oppose each other, and because of rapid ejection of blood, the walls are brought further together by the venturi effect, causing an abrupt cessation in blood flow
- Subsequently the venturi effect subsides as there is no flow, and the systolic pressure is able to overcome the outflow obstruction once more, leading to the second impulse
- As systole progresses and LVOT obstruction increases, this results in a mid-systolic decrease in the pulse
- This is followed by a followed by a secondary increase;
What are the indications for inserting an AICD in a patient with HOCM
- Previous reverted sudden cardiac death
- VF
- Family Hx of sudden cardiac death
- unexplained syncope
- non-sustained VT >3beats at rate >120/m
- Maximal LV wall thickness greater than or equal to 30 mm.
Tetralogy of Fallot
General appearance:
What are the components of tetralogy of fallot?
What are the differential diagnosis?
What are the causes of cyanotic congenital heart disease?
What would an ECG show?
What would a CXR show?
- Cyanotic
- Breathless at rest
- Finger clubbing
- Stigmata of infective endocarditis
- Absent pulse at the site of the blalock-Taussig shunt
- One arm smaller than the other (due to lack of blood supply)
- One arm has BP lower than the other at the site of the blalock-Taussig shunt
- Absent ‘a’ waves due to atrial fibrillation
- Carotid impulse normal
- Evidence of cyanosis
- fetal-alcohol syndrome facies
- CATCH-22 malformations (di-George)
- Thoracotomy scar for the blalock-Taussig shunt
- Other surgical scars may be present
- Thrusting displaced apex beat if there is AR (rare, but due to prolapse of right coronary cusp of aortic valve)
- Parasternal heave
- Pulmonary systolic thrill
- S1 normal
- S2 single (A2) because pulmonary component is inaudible
- Ejection systolic murmur at the left upper sternal edge, accentuated by inspiration
- Early diastolic murmur of AR (in adults)
- Continuous murmur throughout systole and diastole due to presence of blalock-Taussig shunt
What are the components of tetralogy of fallot?
- Overriding aorta
- Right ventricular outflow obstruction
- Right ventricular hypertrophy
- Ventricular septal defect
What are the differential diagnosis?
- Cyanotic congenital heart disease including transposition of the great arteries
- Acyanotic heart disease now with Eisenmenger’s syndrome
What are the causes of cyanotic congenital heart disease?
- Tetralogy of fallots
- Ebsteins anomaly (where the tricuspid valve is abnormally positioned such that part of the right ventricle is atrialised and the remaining RV is small, also there is usually an ASD or PFO which causes right to left shunting)
- Transposition of the great arteries
What would an ECG show?
- Right atrial enlargement (p-pulmonale)
- Right bundle branch block
- Right ventricular strain pattern (ST-T wave changes in V1 – V2)
What would a CXR show?
- Classically it shows a boot shaped heart
Marfan's syndrome
General inspection
Investigations
- narrow and elongated facies
- pectus excavatum or pectus carinatum
- upper segment (crown to pubic symphysis) < 0.85 x lower segment (pubic symphsis to ground)
- arachnodactyly
- joint hypermobility
- arm span > height
- blue sclera
- evidence of lens replacement
- slit lamp examination for lens dislocation
- AR
- MVP
- evidence of aortic dissection
Investigations
- ECHO - look at serial echocardiograms to detect progressive aortic root dilatation