Osteoporosis
Presentation
- Usually in the long case osteoporosis is identified after a minimal trauma fracture - fracture of wrist, hip, vertebrae, ribs are common
- Patient may be asymptomatic
- BMD - Look at T score, osteopenia if -1 to -2.5, osteoporosis if <-2.5
- Ca, PO4 (low in osteomalacia), vit D, PTH
- Type 1 RTA (Distal) - osteomalacia
- Plain X-rays, but insensitive for bone mineral density. Can see evidence of vertebral fractures - crush fractures
- Post-menopausal, because oestrogen decreases RANKL, therefore oestrogen deficiency increases RANKL and signalling + activation + lifespan of osteoclast
- Age of menopause is important to ascertain
- Drugs - anticonvulsants (interfere with Vit D metabolism), thyroxine over replacement, steroids, chronic heparin therapy, lithium, cyclosporine
- Chronic Liver Disease, Chronic Kidney Disease (decreased Vit D activation, secondary hyperparathyroidism), Rheumatoid arthritis
- Malignancy - multiple myeloma, disseminated carcinoma
- Endocrine - hyperparathyroidism, hypogonadism, cushings syndrome, hyperthyroidism
- Smoking (decreases peak bone mass obtained), alcoholism
- Malabsorption states (coeliacs, chrons, gastric bypass)
- Non-pharmacological
- Falls prevention programs, exercise program focusing on strengthening
- Hip protectors for elderly only show evidence in clinical trials - real life clinical uptake is minimal
- Pharmacological
- Primary prevention - NNT = 100, Indication for anti-resorptive therapy only if 10yr fracture risk estimated to be >10%, which is calculated based on age (>70), BMD and falls risk
- Make sure pt vitamin D and Calcium replete - 1200mg req (2 caltrate tablets), Rx Vitamin D only if deficient, in institutionalised adults, if <60nM --> Rx as get falls reduction
- If vitamin D deficient, aim to replace 3000 - 5000 units/d for 6 - 8 weeks
- In post-menopausal women can use HRT --> reduces hip fracture [HR 0.76], increases breast Ca, stroke, PE, CAD
- Bisphosphonates: PO [Alendronate, risedronate, IV = Zoledronate] --> reduces hip and non-hip fractures, but vertebrae > non-vertebrae b/c prevents trabeculae resorption particularly, NOTE zoledronic acid, once yearly IV infusion, caused increase in serious AF! Also GFR >35, Vit D and Ca replete. Delay Rx by 2/52 if fracture.
- ONJ --> caused by impaired healing after tooth extraction with exposed bone 8/52 after extraction, usually after minimum 2y duration Rx, mainly mandible, last stage mx = Sx debridement. Make sure oral health is adequate prior to initation to avoid the need for tooth extraction whilst on bisphosphonate
- Atypical femoral fracture --> stress fracture, usually after 7yr subtrochanteric fracture. Risk ceases after 1yr cessation of bisphosphonate
- Possibility of holiday --> FIT study with alendronate suggested that BMD peak occurs 4-5 y and plateus, and if you take bisphosphonates off, BMD about the same until about 1y.
- Denosumab --> mab against RANKL, acting as OPG does. increases BMD vertebral + non vertebral, decreases fracture rates throughout skeleton, ONJ cases rare [eTG]. ALSO large increases in BMD lost pretty quickly after cessation [cf bisphosphonates]. On PBS as first line Rx
- Teriparatide --> synthetic PTH, if intermittent causes increases osteoblast activity, after 18/12 stimulates osteoclast activity by increased RANK-L and decreased OPG from PTH receptor on osteoblast, gives 18/12 anabolic window. PBS reserved for severe osteoporosis [BMD <-3 AND >=2 Minimal trauma fractures AND 1 fracture despite 12/12 anti-resorptive AND must be only agent AND only for 18/12], black-box warning for osteosarcoma
- Make sure pt vitamin D and Calcium replete - 1200mg req (2 caltrate tablets), Rx Vitamin D only if deficient, in institutionalised adults, if <60nM --> Rx as get falls reduction
- Primary prevention - NNT = 100, Indication for anti-resorptive therapy only if 10yr fracture risk estimated to be >10%, which is calculated based on age (>70), BMD and falls risk
- Surgical
- Fractures may require operative management. Note that bisphosphonate should be started 2/52 after acute fracture
- Vertebroplasty = injecting cement into vertebrae to harden it: "Based upon moderate quality evidence, our review does not support a role for vertebroplasty for treating osteoporotic vertebral fractures in routine practice. We found no demonstrable clinically important benefits compared with a sham procedure and subgroup analyses indicated that results did not differ according to duration of pain ≤ 6 weeks versus > 6 weeks." - cochrane 2015
- Of the disease: fractures, pain, progressive kyphosis, decreased quality of life
- Of treatment: Bisphosphonates --> ONJ, interstitial nephritis, atypical femoral fracture, oesophagitis
Erectile Dysfunction
History
- Risk factors
- Diabetes
- CV Disease/ PVD
- Peripheral Neuropathy
- Prostatectomy
- OSA
- Smoking
- EtOH
- Hypogonadism
- Drugs
- Psychosocial Factors
- Patient Factors
- Partner Expectations
- Depression/Anxiety
- Testosterone
- prolactin level
- BSL for diabetes
- Non-pharmacological
- Counselling
- Education – patient and partner
- Exercise
- Smoking cessation
- Alcohol cessation
- Pharmacological - although only 50% success rates
- Sildenafil (Viagra) – PDE5 inhibitor
- Don’t use with nitrates
- Caution w/ IHD
- Start low dose in elderly 25mg/d
- Use ½ hr before sex
- Can up titrate to max 100mg/d
- Tadanafil (Cialis) – Long-Acting PDE5 inhibitor
- Other:
- Intracavernosal injections of alprostadil, a vasodilator
- Vacuum restriction devices
- Penile prostheses
- Education
- Still need sexual stimulation for drugs to work
- Need adequate trial of drugs
- May need to change drugs
- EtOH/smoking = poor result
- Exercise improves effect
- Sildenafil (Viagra) – PDE5 inhibitor
Diabetes Mellitus
- History
- Type of diabetes
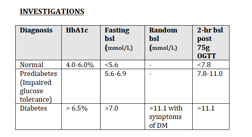
- Diagnosis
- When/ How/ symptoms/ tests
- Monitoring
- Home bsl monitoring pre-meal
- HbA1c
- Hypos and awareness
- Follow up
- Endocrinologist/ GP
- Podiatry – need q3 monthly
- Ophthal – need q12 monthly
- Treatment history and compliance
- Hypoglycaemic events: hypo defined as bsl <4.0, generally develop Sx once <3.5, hypo unawareness often results in 1st Sx at <2.5
- Autonomic symptoms (tremor, palpitations, diaphoresis)
- Neuroglycopenic symptoms (confusion, slurred speech)
- Diet history
- Complications
- Diabetic emergencies
- Microvascular
- Nephropathy: most common cause of CKD, ask about whether they have proteinuria
- Retinopathy: proliferative versus non-proliferative
- Neuropathy:
- Peripheral neuropathy (ulcers and amputations)
- Autonomic neuropathy (Erectile dysfunction, Fainting, Nocturnal diarrhoea)
- Macrovascular
- CVD
- PVD --> ask about Sx of claudication
- CVA
- Associated Metabolic syndrome and PCOS
- Type I – ask about associated autoimmune disease
- Graves/ Hashimoto thyroiditis
- Coeliac
- Addison’s disease
- Vitiligo
- Autoimmune hepatitis
- MG
- Pernicious anaemia
- BMI
- Acanthosis nigricans and skin tags = signs of insulin resistance
- Cardio exam --> failure from previous ischaemia
- Peripheral pulses
- LL neuro exam – monofilament, vibration, reflexes
- Retinopathy
- Non-proliferative
- Dot and blot haemorrhages
- Hard exudates
- Microaneurysms
- Proliferative
- New vessels
- Vitreous haemorrhage
- Non-proliferative
- Insulin injection sites
- Charcot joints (neuropathic arthropathy, most common in foot, presents with collapse of the arch)
- HbA1c, measure every 3 months (can be difficult to interpret in setting of anaemia)
- Type I diabetes
- Islet cell Ab
- Anti insulin Ab
- Anti glutamic acid decarboxylase Ab
- Anti Zn transporter (ZnT8)
- Plasma C-peptide level --> will be low in T1DM due to endogenous insulin deficiency (can be used to differentiate b/w endogenous and exogenous hyperinsulinaemia)
Management of glucose
Non-Pharmacological
- Education: CNC, educator, Diabetes Australia
- Weight loss to increase insulin sensitivity
- Diet - this must be personalised
- Low calorie, high fibre, low fats
- DASH
- Mediterranean diet, especially if there is a past history of stroke
- Epidemiological evidence to increase whole grain consumption BMJ 2016;353:i2716
- Physical activity - aim 150 min/ week moderate activity
- In type 2 diabetic adults, frequent 3-minute exercise breaks lowered glucose and insulin levels Diabetes Care 2016 Jun 39:964
- At diagnosis, if HBA1C < 7 - 7.5%, allow highly motivated patients the opportunity to perform 3 - 6 months of lifestyle modification
- If there is moderate hyperglycaemia or you anticipate lifestyle modification difficulties, just go on to start anti-hyperglycaemic agents
- Goals:
- HbA1c <7 for most patients,
- HbA1c <6.0 if no CVD and only on metformin/ lifestyle
- HbA1c <6.5% if no CVD and on a OHG but NO insulin
- HBa1c <7.0 if on insulin
- HBa1c <8 if previous hypoglycemic events or in older patients with limited life expectancy
- If lifespan limited, then only treatment of symptomatic hyperglycaemia
- In general, metformin is the first line option. It should be started at a low dose with up escalation, because of gastrointestinal side effects.
- If patients Have HBa1c > 9%, achieving satisfactory control with only one agent is probably not going to work, combining two agents is not unreasonable
- There are no good guidelines to suggest an advantage of one agent over an other when advancing to dual oral agents. Initation should be guided by the anticipated side-effects and patients choice
- Metformin (Biguanide) – SEs = diarrhoea, nausea, lactic acidosis, B12 malabsorption
- Weight loss or weight neutral, improves macrovascular outcomes
- Gliclazide (Sulfonylureas) - SEs = hypos, weight gain
- Alpha glucosidase inhibitors - SE = flatulence, abdominal discomfort
- Glitazones - Increased fracture risk, increased MI risk with rosiglitazone
- no hypoglycaemia,
- GLP-1 mimetics
- exanatide - promotes weight loss, SE = nausea, vomiting, possible pancreatitis
- liraglutide
- DPP-4 inhibitors
- sitagliptin (PO tablets) - weight neutral
- SGLT2 inhibitors
- euglycaemic ketoacidicos, urinary tract infections
- NEJM2015 – Empagliflozin compared to placebo decreased primary outcome, death from cardiovascular cause, death from any cause and hospitalization from heart failure
- Insulin
- any insulin product will reduce BGLs and HbA1c
- all insulins will increase wight
- Generally, long-acting insulin analogs reduce the incidence of overnight hypoglycemia, and rapid-acting insulin analogs reduce postprandial glucose excursions as compared with corresponding human insulins (NPH, Regular), but they generally do not result in clinically signifi cantly lower HbA1c.
- Metformin is generally continued as studies demonstrate less weight gain
- Regimens:
- Basal (intermediate/ long) + bolus (short)
- Twice daily Pre-mixed insulin (mix of short and intermediate)
- Insulin Pump
- Continuous infusion of very short acting insulin + mealtime boluses
- Only used in T1DM, studies have shown mild improvement (0.2%) improvement in HbA1c
- Need to carb count
- Starting insulin in T2DM patient:
- Start long acting insulin such as lantus at 10-12U nocte PLUS continue normal OHG
- Increase long insulin on a weekly or second weekly basis. Aim for pre-breakfast fasting bsl of 4-6
- If not achieving goal bsl then change to twice daily pre-mixed insulin
- Need to monitor bsl 4 x per day when on insulin
- Starting basal-bolus regime:
- lantus at 0.2 - 0.25U/kg, increase by 10% weekly - second weekly if fasting BGL > 8, if have hypoglycaemia (< 4), decrease by 20% next dose
- novorapid (or other rapid acting insulin) 0.2 - 0.25U/kg, dividing in three for three meals, immediately before meals, withhold if NBM or on clear fluids
- Troubleshooting: Somogyi effect, where there is a rebound morning hyperglycaemia following nocturnal hypoglycaemia due to release of counter-regulatory hormones - treat by decreasing nocturnal insulin. Dawn effect is early morning hyperglycaemia in absence of nocturnal hypoglycaemia, treat by increasing insulin
- Microalbuminuria
- Type I start monitoring 5 years from diagnosis
- Type II start monitoring at diagnosis
- ACR:
- <3 normal
- 3-30 microalbuminuria
- 30-300 macroalbuminuria
- >300 Nephrotic range proteinuria
- Treat microalbuminuria with an ACE I or ARB
- Once proteinuria is present, progression to ESRF over 5-10yrs is inevitable
- ACE-I/ ARBs Slow progression from microalbuminuria --> macroalbuminuria --> ESKD but does not prevent it
Diabetic Gastroparesis
- Clinical features = bloating, early satiety, nausea and vomiting, post prandial hypoglycaemia
- Confirm Dx with nuclear medicine gastric emptying study
- Treat with prokinetic agent such as metoclopramide or domperidone
Diabetic retinopathy
- Direct ophthalmoscopy +/- Retinal photography performed every 1-2 years. Start at diagnosis of T2DM and 3-5years after diagnosis in T1DM
- If anything other than minimal disease then review every 6-12 months
- Referral to ophthalmologist indicated for:
- Moderate non-proliferative changes
- Proliferative changes
- Macula involvement
Diabetic neuropathy
- Yearly review to look for evidence of neuropathy
- Once found, 3/12 podiatry reviews
Diabetic cardiovascular disease
- Simvastatin 40mg daily reduced the risk of heart attack, stroke and of revascularisation by about one-third (intention to treat)
- Effective irrespective of cholesterol level (or age, sex, or other treatments)
- Use of aspirin as primary prevention is controversial
Hypoglycaemias
- More common in T1 DM due to unstable nature of disease with loss of counter regulatory hormones
- Advise against driving if frequent hypoglycaemias (particularly hypo unawareness) or if significant peripheral neuropathy or if significant retinopathy
How do you manage glycemic control in a patient who is fasting for a procedure?
- All patients with diabetes will need review and adjustment of their usual diabetes management if they need to be fasted for investigations or procedures
- The decision to fast patients with diabetes, and the timing of the fasting, need to be communicated in an effective and timely manner to both the medical team responsible for the patient and the diabetes inpatient service (if involved with that patient’s care) as diabetes management will need prompt review and adjustment anticipating the impact that fasting will have on glucose levels/insulin requirement
- Diabetes medications, other than insulin, should be withheld
- Insulin treated patients :
- Rapid/short-acting insulin should be withheld
- Long-acting basal insulin (eg glargine, detemir) should be continued
- Patients on intermediate acting insulin eg Protaphane, Humulin NPH may have this insulin continued OR changed over to glargine insulin
- Patients on pre-mix insulins should be commenced on glargine insulin - 0.25U/kg if >60kg, or 0.2U/kg if <M60kg, T1DM, CVD
- They involve the full thickness of the dermis of the foot and are often classifed according to the wagner classification system
- Grade 1 - dermis but no underlying tissues
- Grade 2 - deeper, penetrating to ligaments and muscle, but not to bone or abscess formation
- Grade 3 - deep ulcers with cellulitis or abscess formation, often complicated by osteomyelitis
- Grade 4 - ulcers with localised gangrene
- Grade 5 - ulcers with extensive gangrene
How do you prevent diabetic foot ulcers
- most effective measure for protection against major amputation is referral to foot care clinic
- wearing therapeutic footwear
- increasing patient education
What treatments are effective for the treatment of patients with diabetic foot ulceration
- Human skin equivalent applied weekly for a max 5 weeks promotes ulcer healing compared to saline moistened gauze
- pressure off-loading with total contact or non-removable cast for plantar ulcers
- systemic hyperbaric oxygen seems to be effective in treating people with severely infected ulcers
Obesity
History
Examination
Management
- History of weight
- Peak weight
- Previous attempts at weight loss and reasons for failure
- FHx of obesity
- Secondary causes of weight gain:
- Tricyclic Antidepressants
- Antipsychotics
- Cushing’s syndrome and steroids
- Hypothyroidism
- Hypothalamic causes
- GH excess
Examination
- BMI
- 18-25 normal
- 25-30 overweight
- 30-35 obesity (moderate), 35-40 (severe), >40 v. severe
- Waist circumference. Increased risk if:
- Male >94cm
- Women >80cm
- Hip to Waist ratio
- Distribution of fat
- BP and fundi for hypertensive changes
Management
- Set achievable goals
- Weight loss of 5-10% of initial weight
- Improved control of DM
- Non-pharmacological
- Diet
- Very Low Calorie Diet - Limit calorie intake to <1200 per day
- Mediterranean diet --> shown to reduce CVD, Olive oil (monounsaturated fat), Rich in fish, fruit and vegetables
- Exercise
- Aim for 30min exercise 5 times per week, Increase incidental exercise, Reduce sedentary time, e.g. screen time
- Can use pedometer to monitor number of steps per day, need >10 000 for weight loss
- Refer to a metabolic clinic for multidisciplinary approach
- Dietician
- Physiotherapist
- Endocrinologist
- Orlistat
- Intestinal lipase inhibitor
- SEs = steatorrhoea
- Phentermine (Duromine)
- Sympathomimetic - an appetite suppressant
- Contraindicated if existing cardiac disease
- Topiramate
- Appetite suppressant
- Not on PBS for this indication
- If has impaired glucose tolerance then metformin has been shown to decrease chance of progression to T2DM (Diabetes Prevention Program study)
- Diabetic management - Use weight neutral agents
- Indication:
- BMI > 40, OR
- BMI 35-40 with significant other disease such as HTN or DM or OSA
- Providing that all appropriate non-surgical weight loss measures have failed
- Types:
- Gastric banding
- Sleeve gastrectomy
- Roux-en-Y Gastric Bypass
- Greater weight loss
- Best at reversing diabetes, increased GLP-1 secretion
- More complications (bowel obstruction = early, anastamotic strictures = late)
- Complications
- Nutritional deficiency.
- NASH flare
- Management post surgery:
- Multivitamin including trace elements
- Vitamin D
- Thiamine (vitamin B1)
- B12 – can replace IM monthly
- Fe deficiency
- Monitor fat-soluble vitamins (A, D, E, K) levels as well as Fe studies, B12, folate and vitamin D. Also monitor LFTs
Hypercalcaemia
History
Primary hyperparathyroidism
- Symptoms: ‘stones, bones, abdo moans, psychic groans’
- CNS (psychic moans) – Tiredness, weakness, confusion episodes,
- GI – constipation, anorexia, nausea and vomiting, acute abdominal pain from pancreatitis, peptic ulcer
- Renal – stones, polyuria, polydypsia - nephrogenic diabetes insipidus
- Cardiac – shortened QT, bradycardia, hypertension
- Joint pain – pseudogout
- Aetiology:
- Hyperparathyroidism
- Primary - Autonomous, spontaneous overproduction of PTH
- Secondary - the parathyroid glands appropriately respond to reduced levels of Ca by increasing PTH synthesis
- Tertiary - Autonomous overproduction of PTH can occur in renal failure after many years of secondary hyperparathyroidism
- Bone metastasis
- Multiple myeloma
- Osteosarcoma
- Sarcoidosis --> macrophages release calcitriol
- Drugs – thiazides, lithium, Ca and Vit D
- Familial hypocalciuric hypercalcaemia (FHH) --> autosomal dominant condition, look for low 24 h urine [calcium]
- Hyperparathyroidism
- Neck scars – previous thyroid/ parathyroid surgery
- Forearm scars – from reimplantation of PTH glands
- Evidence of malignancy – eg LN/ organomegaly
- Renal failure sx
- Resp system – evidence of sarcoid, Tb or histoplasmosis
- HR – assess for bradycardia
- Proximal weakness
- Joints for pseudogout
- Corneal exam for band keratopathy (at 3 and 9 o’clock)
- Serum Ca
- Sx of hyperCa develop when serum level is >3, once >4 cardiac arrest and coma an occur
- PTH level
- If elevated primary hyperPTH is most likely
- If PTH is low consider:
- FHH
- Hypervitaminosis D
- Sarcoidosis
- Multiple myeloma --> normal ALP suggests MM
- Bone metastases --> raised ALP suggests bone mets
- ALP ( ALP elevated in osteomalacia/ Pagets/ Ca)
- 24 hour urine Ca for FHH
- 25(OH) Vit D, 1, 25 (OH) Vit D
- If malignancy suspected, EPG, IEPG, urine EPG, CT CAP
Primary hyperparathyroidism
- Bisphosphonates
- Calcimimetics such as cinacalcet
- Surgical parathyroidectomy
- Preoperative localization is not required for most surgeons however can do USS, CT or sestamibi (w technetium 99)
- Need to supplement life long Vit D after surgery (if HypoCa), or reimplant tissue in the arm
- Treat underlying tumour
- IVF – aggressive, with frusemide to treat fluid overload
- Bisphosphonates – need repeat doses. Eg IV zoledronate/ palmidronate
- Steroids can help
- IV calcitonin – only transient effect
- Lithium treatment – may need to cease, note doesn't nec mean Li toxicity
Management of long-term complications of corticosteroid use
" I am concerned about the impact of corticosteroids on Mr RW's general health. In particular, I am concerned about his future risk of developing glucocorticoid induced diabetes, osteoporosis and proximal myopathy which may threaten his already vulnerable mobility"
What are the most common side effects of glucocorticoids when used in the long term?
How would you manage his bone health in the face of anticipated corticosteroid use?
How should you manage the risk of adrenal supression due to supra-physiological glucocorticoid use?
How would you manage the risk of steroid induced diabetes?
What is an appropriate tapering regime for patients who are at risk or who have evidence of HPA-axis suppression?
What are the most common side effects of glucocorticoids when used in the long term?
- osteoporosis and fractures
- HPA-axis suppression
- Cushingoid appearance and weight gain
- hyperglycemia/diabetes
- CVD and dyslipidemia
- myopathy
- cataracts and glaucoma
- psychiatric disturbances
- immunosuppression
- other GI and dermatologic events
How would you manage his bone health in the face of anticipated corticosteroid use?
- Annual height measurement
- Assessment of BMD at baseline and after 1 year of glucocorticoid therapy if receiving >5mg/d
- Maintain optimal calcium and vitamin D levels, Calcium intake should be >1200mg/d
- For glucocorticoids BMD cut-off = <-1.5 for the initation of anti-resorptive therapy. Fracture risk starts at time of initiation
- Teriparatide has been shown to be effective in improving BMD and reducing vertebral fractures in patients with GC-induced osteoporosis
- Denosumab is not currently recommended as first line
- As soon as possible, reduce corticosteroid use to minimise risk
How should you manage the risk of adrenal supression due to supra-physiological glucocorticoid use?
- The risk of AS is low in patients who have been treated with GC therapy for less than 1 week
- Based on current evidence, experts recommend that physicians be aware of the risk of AS in patients receiving supraphysiological GC doses for >2 weeks, those who have received multiple courses of oral steroids totaling >3 weeks in the last 6 months, or in patients presenting with symptoms of AS
- If you are not sure if adrenal suppression is present --> check early AM cortisol, if lower than the lower limit of normal (provided that the evening and morning doses have been held) then may need tapering dose. But the presence of a normal value does not rule it out
- Confirmatory testing with short synacthen test can be used
- Consider stress dose steroids
How would you manage the risk of steroid induced diabetes?
- Ask patients to monitor for symptoms of hyperglycaemia
- ALL patients commenced on steroids should have BGLs checked before breakfast and 2 hours postprandially after lunch and after dinner on Day 3 after starting them and then at least weekly using the same daily blood glucose monitoring regimen thereafter if the steroid dose is still above prednisone 15mg daily or dexamethasone 2mg daily
- Initial management involves appropriate lifestyle modification strategies; if targets are not met with these modifications, pharmacotherapy is recommended, and the same spectrum of glucose-lowering medications is used for GC-induced diabetes as is used for pre-existing type 2 diabetes.
- If blood glucose levels are <15 mmol/L, then glucose control can likely be achieved with non-insulin therapies
- If blood glucose levels are >15 mmol/L, then insulin is usually required to achieve glycemic control. In the absence of a contraindication, metformin is often recommended in combination with insulin
- Intermediate acting insulins should be utilised due to the activity profile of corticosteroids
- Morning doses of glucocorticoid such as prednisone lead to postprandial hyperglycaemia with BGLs usually highest between 1200-2000 hours and then fall overnight so an appropriate insulin regimen is needed to have maximal effect from1200-2000 hours
- Other glucocorticoid regimens or long-acting steroids eg dexamethasone will lead to different patterns of hyperglycaemia and need tailored insulin regimens
- Endocrinology advice is required
- The following insulin regime is applied at RPAH
- Pre-breakfast Protaphane Insulin (initiate/adjust according to pre-lunch BGL)
- Pre-lunch Actrapid Insulin (initiate/adjust according to 2hr [post-lunch BGL)+ pre-lunch Protaphane Insulin (initiate/adjust according to pre-dinner BGL)
- Pre-dinner Actrapid insulin may be needed to control post dinner BGLs but it is not always needed
- Patients usually on evening/pre-bed Lantus/Protaphane insulin before receiving steroids could be continued on it as well (minor dose adjustment may be needed)
What is an appropriate tapering regime for patients who are at risk or who have evidence of HPA-axis suppression?
- Reduce dose by 2.5- to 5.0-mg decrements every 3–7 days until physiologic dose (5 to 7.5 mg of prednisone per day) is reached; slower tapering of GC therapy may be recommended if risk of disease relapse is a concern
- Then switch to hydrocortisone 20mg mane
- Gradually reduce hydrocortisone by 2.5mg over weeks to months and re-assess based on morning cortisol, and if required, ACTH simulation test
Paget's disease
General information
- Pathophysiology relates to focal areas of increased and disorganised bone remodelling
- targets axial skeleton, pelvis (70%), femur (55%), lumbar spine (53%), skull (42%), tibia (32%)
- upto 8% affected >80, rare <55y
- Probably has genetic basis
- only 30 - 40% have symptoms at time of diagnosis
- Usually asymptomatic
- isolated raised ALP (bone specific ALP more specific) with concomitant radiological abnormalities
- bone pain most common sx
- increased bone turnover
- secondary OA of affected joint
- spinal stenosis
- pseudofracture
- deafness if involvement of skull - can be conductive or sensorineural
- Rare complications
- osteosarcoma a rare complication
- obstructive hydrocephalus
- high output cardiac failure
- hypercalcaemia
- bone deformity - bowing of legs, skull changes
- high output cardiac failure
- bone bruits
- erythema over site of bony lesion
- fundoscopy - angiod streaks etc
- Radiography - focal osteolysis, coarsening of trabeculae, bone expansion, cortical thickening
- Bone radionucleotide scans - show extent of disease
- Alkaline phosphatase, especially bone specific alkaline phosphatase which more closely parallels disease activity
- Symptom relief with analgesia
- If bone pain then there is indication for antiresorptive Rx
- no evidence that asymptomatic pts benefit
- bone pain caused by increased metabolic activity
- best bisphosphonates are nitrogen containing bisphosphonates - alendronate, risedronate, pamidronate and zoledronic acid
- levels of ALP begin to fall after 10 days of initiating therapy