Question 1
Which of the following is not a contraindication to thrombolysis for acute ischaemic stroke?
(A) patient awoke with weakness, however when last seen by spouse five hours earlier, was neurologically normal
(B) BP >185/110 mmHg, non responsive to antihypertensives, at intended time of lysis
(C) Radiological evidence of > 1/3 middle cerebral artery territory
(D) INR >1.7
(E) Platelets < 150
E: platelet count <100
Question 2
What is the lifetime prevalence of stroke?
(A) 1:100
(B) 1:48
(C) 1:18
(D) 1:6
(E) 1:3
D: 85% of strokes are ischaemic, of which the vast majority are cardio-embolic. Only 15% of strokes are hemorrhagic, of which 75% are intracerebral haemorrhage and 25% subarachnoid.
Question 3
A 32 year old male presents to ED at 11pm with a sudden onset headache 4 hours earlier. She describes the event as suddenly being hit on the head. Subsequent to this she experienced an ongoing sudden severe occipital headache and vomiting. The provisional diagnosis of a subarachnoid haemorrhage is made. CT scanning however is unyielding. What is the most appropriate next step in the management?
(A) arrange an urgent MRI brain
(B) Address his analgesic requirements and discharge him after pain control is sufficient
(C) Perform a lumbar puncture and CSF for xanthochromia immediately
(D) Perform a lumbar puncture and CSF for xanthochromia the next morning
(E) Observe him in hospital and arrange repeat CT brain the next day
D: An MRI has a sensitivity similar to that of a CT, therefore a negative MRI in this instance would still result in the patient having to progress to a lumbar puncture. 12 hours have to elapse prior to undertaking LP for the detection of xanthochromia. Under these conditions the sensitivity of this test is greater than 95%. Stroke. 2012 Jun;43(6):1711-37
Question 4
With regards to the treatment of subarachnoid haemorrhages, what is FALSE?
(A) Coiling achieves more superior outcomes than clipping in terms of mortality
(B) Coiling is associated with more re-bleeding rates
(C) Blood pressure should be kept to a level <160mmHg
(D) Nifedipine should be used within 4 days and to a total of 21 days post index event
(E) Hydrocephalus should be suspected in any patient with neurological deterioration, and this should be treated with a ventricular shunt
D: Nimodipine is favoured, and has been shown to improve neurological outcomes when used in this situation acutely. Coiling has less mortality but greater re-bleeding rates. The dose is nimodipine 60mg QID. The original hypothesis is that it prevented cerebral vasoconstriction however this is only speculative. N Engl J Med. 1983;308(11):619, J Neurosurg. 1988;68(4):505. BMJ. 1989;298(6674):636.
Question 5
What is the most common stroke mimic?
(A) seizure
(B) migraine
(C) cluster headache
(D) meaning-encephalitis
(E) arteriovenous malformation
A: 23% (RPA course 2015)
Question 6
A 68 year old chinese male presents to the emergency department with a right facial droop that spares his nano-labial folds with associated speech changes. He makes a spontaneous recovery within 4 minutes. His blood pressure is 168/98. His LDL cholesterol is 1.75, with total cholesterol 4.3. A CT-B and CT-A are normal, as are MRI diffusion weighted images. An EEG shows a normal background posterior rhythm. Hotter monitor did not show any evidence of AF. What is the most appropriate management for this patient?
(A) clopidogrel + statin + ace-inhibitor + no-driving for 2 weeks
(B) Aspirin + dipyridamole + statin + ace-inhibitor + no-driving for 2 weeks
(C) aspirin + clopidogrel + statin + ace-inhibitor + no-driving for 2 weeks
(D) aspirin + clopidogrel + ace-inhibitor + no-driving for 2 weeks
(E) clopidogrel + ace-inhibitor + no-driving for 2 weeks
C: In chinese patients, the ARR of adding aspirin and clopidogrel as anti-thrombotic therapies was beneficial (ARR 3.5%) over aspirin alone, only if followed for 3 weeks then changed to clopidogrel mono therapy. Regardless of the lipid levels, a statin should be prescribed. Blood pressure should be reduced to < 140/90, however there is now mounting evidence for greater cardiovascular outcomes of blood pressure <120/80 as per the SPRINT trial - but the results did not include diabetic patients. N Engl J Med 2013; 369:11-19; November 9, 2015DOI: 10.1056/NEJMoa1511939 - SPRINT trial; N Engl J Med 2012; 366:1914-1922
Question 7
Which group of patients would most benefit from carotid endarterectomy?
(A) Patient who is 4 weeks post acute CVA with 80% carotid stenosis
(B) Patient who has intracranial atherosclerotic lesion causing flow limitation on digital subtraction angiography
(C) Patient who is 2 weeks post acute CVA with 80% carotid stenosis
(D) Patient who is 2 weeks post acute CVA with 100% carotid stenosis
(E) Patient who is asymptomatic with 95% carotid stenosis
C: If the patient is asymptomatic then there is no evidence for surgical intervention. Endarterectomy is preferred over stenting, however there may be some evidence in young patients for stunting (evidence evolving, CREST trial). There is no evidence for a fully completed carotid occlusion. N Engl J Med 2013; 369:1143-1150; N Engl J Med 2010;363:11-23; [Erratum, N Engl J Med 2010;363:198, 498.]
Question 8
A 64 year old male with a past history of type 2 diabetes presents to the ED 3 hours after noticing a dense right sided weakness. His partner also noted him to have eye deviation to the left side. He had surgery 7 months ago to repair an inguinal hernia. He has no bleeding diathesis. Examination reveals expressive aphasia with concomitant right sided dense motor-sensory deficit. Blood pressure is 145/76. His NIIHS score is 23. A CT brain is reported as normal. Blood tests reveal an INR of 1.6 and platelet count of 142. What is the most appropriate management?
(A) TPA after consent + further brain imaging to determine suitability for clot retrieval as within the 6 hour window period
(B) TPA after consent
(C) TPA contra-indicated due to elevated INR
(D) TPA contra-indicated due to mild thrombocytopenia
(E) no TPA, pursue brain imaging and if suitable, retrieve clot
A: Standard of care at facilities that can offer this service. N Engl J Med 2015; 372:2285-2295 (reduced modified rankin scores at 90 days but no mortality difference - SWIFT PRIME); N Engl J Med 2015; 372:11-20 (MR CLEAN - same results as SWIFT PRIME); N Engl J Med 2015; 372:1019-1030 (Australian trial --> mortality was reduced 10% cf 19% control if selected based on collateral and infarct core size where large infarct core and/ or poor collateral circulation excluded).
Question 9
A 74 year old male presents to the emergency department with symptoms consistent with a left sided MCA stroke. There is no significant oedema or mass shift or haemorrhage on initial CT scan, however there is a large infarct size > 1/3 of MCA territory. A decision of not to thrombolyse is made given the imaging findings. A hotter monitor however reveals the patient has atrial fibrillation. What is the most appropriate management
(A) Initiate aspirin + clopidogrel + NOAC straight away
(B) Initiate NOAC 2 weeks after incident
(C) Initiate warfarin 2 weeks after incident
(D) Observe patient for further events
(E) Initiate aspirin OR aspirin + clopidogrel OR clopidogrel OR aspirin + dipyrimadole
B: Dabigatran at 150mg BD has superiority over warfarin in terms of stroke prevention, but with similar bleeding rates. 110mg BD dossing is non-inferior to warfarin with lower bleeding rates. Gastrointestinal bleeding was higher with the NOACs, and the agents shouldn't be used if CrCL <30 (apixaban may be used if CrCl >= 25). Australian guidelines say that up to 2 weeks delay in initiating anti-coagulation therapy is reasonable. N Engl J Med 2009; 361:1139-1151. However, if the patient had valvular AF, then NOACS have no place and can actually do harm (increased risk of bleeding and thromboembolic complications) N Engl J Med 2013; 369:1206-1214.
Question 10
Which of the following is FALSE regarding the management of acute ischaemic stroke?
(A) All patients should be admitted to a stroke ward
(B) Patient should be advised not to drive for one month
(C) Heparin prophylaxis is equivalent to enoxaparin prophylaxis
(D) Implantable cardiac monitors are better than hotter monitors for detecting AF
(E) A thorough such for an underlying aetiology should be sought after
C: clexane is greater than heparin with respect to DVT prophylaxis (RPA lectures 2015, RPA course 2015)
Question 11
What is the rate of chiropractic neck manipulations that result in a carotid or vertebral artery dissection?
(A) 1: 1000
(B) 1: 10000
(C) 1: 20000
(D) 1: 50000
(E) 1: 100000
C: This is at least 5 - 10x the population rate ( 2.5 - 3/ 100 000). This however may be an over-estimation of the true value because 25% of these patients actually had connective tissue diseaseand the initial symptoms of vertebral-artery dissection commonly mimic the musculoskeletal neck pain for which people go to chiropractors N Engl J Med 2001; 344:898-906.
Question 12
What symptom is NOT typically associated with dissection of the internal carotid artery?
(A) unilateral headache
(B) Ptosis
(C) Miosis
(D) Anhydrosis
(E) cranial nerve palsies
D: Oculosympathetic palsy, consisting of miosis and ptosis, has long been recognized as a typical manifestation of carotid-artery dissection, but it is found in less than half of patients. Facial anhidrosis is not present because the facial sweat glands are innervated by the sympathetic plexus surrounding the external carotid artery. Cranial-nerve palsies can be detected in about 12 percent of patients with carotid-artery dissection. The lower cranial nerves are the most commonly affected, particularly the hypoglossal nerve, and the involvement of various combinations of nerves has been described. N Engl J Med 2001; 344:898-906.
Question 13
Which of the following is a recognised treatment option for carotid or vertebral artery dissection?
(A) Aspirin
(B) therapeutic anticoagulation
(C) intralesional tPA
(D) endoluminal thrombectomy
(E) high dose atorvastatin
B: One approach is to anticoagulate initially with UFH then bridge to warfarin therapy, maintaining INR 2.0 - 3.0. Subsequent to this MRA can be performed, and if there are further luminal irregularities then anticoagulation may continue for a further 3 months. N Engl J Med 2001; 344:898-906
Question 14
A 64 year old female with poorly controlled hypertension presents acutely with sudden flinging movements of her left arm and leg. This movement has caused her to injure her left leg. An MRI of her brain would most likely reveal a lesion in which of the following sub-cortical structures?
(A) Subthalamic nucleus
(B) Globus pallidus internen
(C) Globus pallidus externen
(D) Caudate nucleus
(E) Putamen
A: It is widely acknowledged that the majority of causes of hemiballismus occurs due to lesions in the subthalamic nucleus on the contralateral side to the deficit. The most common aetiology being hypertensive disease, however inflammatory plaques from diseases such as multiple sclerosis may also cause a similar picture. Other aetiologies include non-ketotic hyperglycaemia, and when pharmacological treatment is necessary, haloperidol, chlorpromazine and topiramate has been used. Lancet Neurol 2006; 5:589. J Neurol 2004; 251:725.
Question 15
A 58-year-old man was admitted with a history of occipital headache of sudden onset associated with nausea, vomiting, vertigo, double vision and slurred speech. On examination, he was confused and had mild dysarthria. There was no neck stiffness. He had normal tone and power in his limbs with normal reflexes. Sensation seemed normal but was hard to assess because of his confusion. A CT scan was performed (radiopedia.org)
Which of the following is not a contraindication to thrombolysis for acute ischaemic stroke?
(A) patient awoke with weakness, however when last seen by spouse five hours earlier, was neurologically normal
(B) BP >185/110 mmHg, non responsive to antihypertensives, at intended time of lysis
(C) Radiological evidence of > 1/3 middle cerebral artery territory
(D) INR >1.7
(E) Platelets < 150
E: platelet count <100
Question 2
What is the lifetime prevalence of stroke?
(A) 1:100
(B) 1:48
(C) 1:18
(D) 1:6
(E) 1:3
D: 85% of strokes are ischaemic, of which the vast majority are cardio-embolic. Only 15% of strokes are hemorrhagic, of which 75% are intracerebral haemorrhage and 25% subarachnoid.
Question 3
A 32 year old male presents to ED at 11pm with a sudden onset headache 4 hours earlier. She describes the event as suddenly being hit on the head. Subsequent to this she experienced an ongoing sudden severe occipital headache and vomiting. The provisional diagnosis of a subarachnoid haemorrhage is made. CT scanning however is unyielding. What is the most appropriate next step in the management?
(A) arrange an urgent MRI brain
(B) Address his analgesic requirements and discharge him after pain control is sufficient
(C) Perform a lumbar puncture and CSF for xanthochromia immediately
(D) Perform a lumbar puncture and CSF for xanthochromia the next morning
(E) Observe him in hospital and arrange repeat CT brain the next day
D: An MRI has a sensitivity similar to that of a CT, therefore a negative MRI in this instance would still result in the patient having to progress to a lumbar puncture. 12 hours have to elapse prior to undertaking LP for the detection of xanthochromia. Under these conditions the sensitivity of this test is greater than 95%. Stroke. 2012 Jun;43(6):1711-37
Question 4
With regards to the treatment of subarachnoid haemorrhages, what is FALSE?
(A) Coiling achieves more superior outcomes than clipping in terms of mortality
(B) Coiling is associated with more re-bleeding rates
(C) Blood pressure should be kept to a level <160mmHg
(D) Nifedipine should be used within 4 days and to a total of 21 days post index event
(E) Hydrocephalus should be suspected in any patient with neurological deterioration, and this should be treated with a ventricular shunt
D: Nimodipine is favoured, and has been shown to improve neurological outcomes when used in this situation acutely. Coiling has less mortality but greater re-bleeding rates. The dose is nimodipine 60mg QID. The original hypothesis is that it prevented cerebral vasoconstriction however this is only speculative. N Engl J Med. 1983;308(11):619, J Neurosurg. 1988;68(4):505. BMJ. 1989;298(6674):636.
Question 5
What is the most common stroke mimic?
(A) seizure
(B) migraine
(C) cluster headache
(D) meaning-encephalitis
(E) arteriovenous malformation
A: 23% (RPA course 2015)
Question 6
A 68 year old chinese male presents to the emergency department with a right facial droop that spares his nano-labial folds with associated speech changes. He makes a spontaneous recovery within 4 minutes. His blood pressure is 168/98. His LDL cholesterol is 1.75, with total cholesterol 4.3. A CT-B and CT-A are normal, as are MRI diffusion weighted images. An EEG shows a normal background posterior rhythm. Hotter monitor did not show any evidence of AF. What is the most appropriate management for this patient?
(A) clopidogrel + statin + ace-inhibitor + no-driving for 2 weeks
(B) Aspirin + dipyridamole + statin + ace-inhibitor + no-driving for 2 weeks
(C) aspirin + clopidogrel + statin + ace-inhibitor + no-driving for 2 weeks
(D) aspirin + clopidogrel + ace-inhibitor + no-driving for 2 weeks
(E) clopidogrel + ace-inhibitor + no-driving for 2 weeks
C: In chinese patients, the ARR of adding aspirin and clopidogrel as anti-thrombotic therapies was beneficial (ARR 3.5%) over aspirin alone, only if followed for 3 weeks then changed to clopidogrel mono therapy. Regardless of the lipid levels, a statin should be prescribed. Blood pressure should be reduced to < 140/90, however there is now mounting evidence for greater cardiovascular outcomes of blood pressure <120/80 as per the SPRINT trial - but the results did not include diabetic patients. N Engl J Med 2013; 369:11-19; November 9, 2015DOI: 10.1056/NEJMoa1511939 - SPRINT trial; N Engl J Med 2012; 366:1914-1922
Question 7
Which group of patients would most benefit from carotid endarterectomy?
(A) Patient who is 4 weeks post acute CVA with 80% carotid stenosis
(B) Patient who has intracranial atherosclerotic lesion causing flow limitation on digital subtraction angiography
(C) Patient who is 2 weeks post acute CVA with 80% carotid stenosis
(D) Patient who is 2 weeks post acute CVA with 100% carotid stenosis
(E) Patient who is asymptomatic with 95% carotid stenosis
C: If the patient is asymptomatic then there is no evidence for surgical intervention. Endarterectomy is preferred over stenting, however there may be some evidence in young patients for stunting (evidence evolving, CREST trial). There is no evidence for a fully completed carotid occlusion. N Engl J Med 2013; 369:1143-1150; N Engl J Med 2010;363:11-23; [Erratum, N Engl J Med 2010;363:198, 498.]
Question 8
A 64 year old male with a past history of type 2 diabetes presents to the ED 3 hours after noticing a dense right sided weakness. His partner also noted him to have eye deviation to the left side. He had surgery 7 months ago to repair an inguinal hernia. He has no bleeding diathesis. Examination reveals expressive aphasia with concomitant right sided dense motor-sensory deficit. Blood pressure is 145/76. His NIIHS score is 23. A CT brain is reported as normal. Blood tests reveal an INR of 1.6 and platelet count of 142. What is the most appropriate management?
(A) TPA after consent + further brain imaging to determine suitability for clot retrieval as within the 6 hour window period
(B) TPA after consent
(C) TPA contra-indicated due to elevated INR
(D) TPA contra-indicated due to mild thrombocytopenia
(E) no TPA, pursue brain imaging and if suitable, retrieve clot
A: Standard of care at facilities that can offer this service. N Engl J Med 2015; 372:2285-2295 (reduced modified rankin scores at 90 days but no mortality difference - SWIFT PRIME); N Engl J Med 2015; 372:11-20 (MR CLEAN - same results as SWIFT PRIME); N Engl J Med 2015; 372:1019-1030 (Australian trial --> mortality was reduced 10% cf 19% control if selected based on collateral and infarct core size where large infarct core and/ or poor collateral circulation excluded).
Question 9
A 74 year old male presents to the emergency department with symptoms consistent with a left sided MCA stroke. There is no significant oedema or mass shift or haemorrhage on initial CT scan, however there is a large infarct size > 1/3 of MCA territory. A decision of not to thrombolyse is made given the imaging findings. A hotter monitor however reveals the patient has atrial fibrillation. What is the most appropriate management
(A) Initiate aspirin + clopidogrel + NOAC straight away
(B) Initiate NOAC 2 weeks after incident
(C) Initiate warfarin 2 weeks after incident
(D) Observe patient for further events
(E) Initiate aspirin OR aspirin + clopidogrel OR clopidogrel OR aspirin + dipyrimadole
B: Dabigatran at 150mg BD has superiority over warfarin in terms of stroke prevention, but with similar bleeding rates. 110mg BD dossing is non-inferior to warfarin with lower bleeding rates. Gastrointestinal bleeding was higher with the NOACs, and the agents shouldn't be used if CrCL <30 (apixaban may be used if CrCl >= 25). Australian guidelines say that up to 2 weeks delay in initiating anti-coagulation therapy is reasonable. N Engl J Med 2009; 361:1139-1151. However, if the patient had valvular AF, then NOACS have no place and can actually do harm (increased risk of bleeding and thromboembolic complications) N Engl J Med 2013; 369:1206-1214.
Question 10
Which of the following is FALSE regarding the management of acute ischaemic stroke?
(A) All patients should be admitted to a stroke ward
(B) Patient should be advised not to drive for one month
(C) Heparin prophylaxis is equivalent to enoxaparin prophylaxis
(D) Implantable cardiac monitors are better than hotter monitors for detecting AF
(E) A thorough such for an underlying aetiology should be sought after
C: clexane is greater than heparin with respect to DVT prophylaxis (RPA lectures 2015, RPA course 2015)
Question 11
What is the rate of chiropractic neck manipulations that result in a carotid or vertebral artery dissection?
(A) 1: 1000
(B) 1: 10000
(C) 1: 20000
(D) 1: 50000
(E) 1: 100000
C: This is at least 5 - 10x the population rate ( 2.5 - 3/ 100 000). This however may be an over-estimation of the true value because 25% of these patients actually had connective tissue diseaseand the initial symptoms of vertebral-artery dissection commonly mimic the musculoskeletal neck pain for which people go to chiropractors N Engl J Med 2001; 344:898-906.
Question 12
What symptom is NOT typically associated with dissection of the internal carotid artery?
(A) unilateral headache
(B) Ptosis
(C) Miosis
(D) Anhydrosis
(E) cranial nerve palsies
D: Oculosympathetic palsy, consisting of miosis and ptosis, has long been recognized as a typical manifestation of carotid-artery dissection, but it is found in less than half of patients. Facial anhidrosis is not present because the facial sweat glands are innervated by the sympathetic plexus surrounding the external carotid artery. Cranial-nerve palsies can be detected in about 12 percent of patients with carotid-artery dissection. The lower cranial nerves are the most commonly affected, particularly the hypoglossal nerve, and the involvement of various combinations of nerves has been described. N Engl J Med 2001; 344:898-906.
Question 13
Which of the following is a recognised treatment option for carotid or vertebral artery dissection?
(A) Aspirin
(B) therapeutic anticoagulation
(C) intralesional tPA
(D) endoluminal thrombectomy
(E) high dose atorvastatin
B: One approach is to anticoagulate initially with UFH then bridge to warfarin therapy, maintaining INR 2.0 - 3.0. Subsequent to this MRA can be performed, and if there are further luminal irregularities then anticoagulation may continue for a further 3 months. N Engl J Med 2001; 344:898-906
Question 14
A 64 year old female with poorly controlled hypertension presents acutely with sudden flinging movements of her left arm and leg. This movement has caused her to injure her left leg. An MRI of her brain would most likely reveal a lesion in which of the following sub-cortical structures?
(A) Subthalamic nucleus
(B) Globus pallidus internen
(C) Globus pallidus externen
(D) Caudate nucleus
(E) Putamen
A: It is widely acknowledged that the majority of causes of hemiballismus occurs due to lesions in the subthalamic nucleus on the contralateral side to the deficit. The most common aetiology being hypertensive disease, however inflammatory plaques from diseases such as multiple sclerosis may also cause a similar picture. Other aetiologies include non-ketotic hyperglycaemia, and when pharmacological treatment is necessary, haloperidol, chlorpromazine and topiramate has been used. Lancet Neurol 2006; 5:589. J Neurol 2004; 251:725.
Question 15
A 58-year-old man was admitted with a history of occipital headache of sudden onset associated with nausea, vomiting, vertigo, double vision and slurred speech. On examination, he was confused and had mild dysarthria. There was no neck stiffness. He had normal tone and power in his limbs with normal reflexes. Sensation seemed normal but was hard to assess because of his confusion. A CT scan was performed (radiopedia.org)
(A) cerebellar infarct
(B) basilar artery thrombosis
(C) middle cerebral artery thrombosis
(D) multiple sclerosis
(E) progressive multifocal leuokoencephalopathy
B: You can clearly see the tip of the basilar artery involved. The most common symptoms include hemiparesis/ tetraperesis and facial paresis, speech involvement is common with dysarthria (as it involves the nucleus ambiguous), visual disturbances due to the involvement of the posterior cerebral hemispheres, vertigo due to involvement of the cerebellum and headache. Altered consciousness may occur due to involvement of the reticular activating system. Sensory loss may also occur due to thalamic involvement. Vertical gaze paralysis occurs because of involvement of mid brain tegmentum. Somnolence is well described in the top of the basilar syndrome. Neurology 1980; 30: 72 - 79
Question 16
What is not associated with bilateral parietal lobe involvement, known as Baliant syndrome?
(A) optic ataxia
(B) optic apraxia
(C) simultanagnosia
(D) headache
(E) left right finger disorientation
E: "Baliant syndrome results from damage to both parietal lobes. Clinically, it includes three main symptoms: simultanagnosia (the inability to see more than one object at a time); optic ataxia (the fixation of gaze with severe problems in voluntarily moving fixation); and optic apraxia (the inability to reach towards the correct location of perceived objects" It can occur with dementia. Balint's syndrome lose spatial information outside their own bodies and are functionally blind except for the perception of one object in the visual scene at a time. Their spatial abilities are so impaired that they cannot locate the item they can perceive." Nature Reviews Neuroscience 2003 4, 93-102
Question 17
The Re-LY stroke trial examined the efficacy of dabigatran compared to warfarin in the prevention of thromboembolic stroke in patients who have atrial fibrillation. Which of the following results was not an outcome from that study?
(A) 110mg BD dabigatran and 150mg BD dabigatran showed a statistically significant decrease in risk of hemorrhagic stroke
(B) 110mg BD dabigatran showed a statistically significant decrease in major bleeding risk, whilst 150mg BD dabigatran showed a similar major bleeding risk when compared to warfarin
(C) 110mg BD dabigatran was found superior to warfarin in prevention of thromboembolic stroke
(D) 150mg BD dabigatran was found superior to warfarin in prevention of thromboembolic stroke
(E) 110mg BD dabigatran was non-inferior to warfarin in prevention of thromboembolic stroke
C: Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361:1139–1151.
(B) basilar artery thrombosis
(C) middle cerebral artery thrombosis
(D) multiple sclerosis
(E) progressive multifocal leuokoencephalopathy
B: You can clearly see the tip of the basilar artery involved. The most common symptoms include hemiparesis/ tetraperesis and facial paresis, speech involvement is common with dysarthria (as it involves the nucleus ambiguous), visual disturbances due to the involvement of the posterior cerebral hemispheres, vertigo due to involvement of the cerebellum and headache. Altered consciousness may occur due to involvement of the reticular activating system. Sensory loss may also occur due to thalamic involvement. Vertical gaze paralysis occurs because of involvement of mid brain tegmentum. Somnolence is well described in the top of the basilar syndrome. Neurology 1980; 30: 72 - 79
Question 16
What is not associated with bilateral parietal lobe involvement, known as Baliant syndrome?
(A) optic ataxia
(B) optic apraxia
(C) simultanagnosia
(D) headache
(E) left right finger disorientation
E: "Baliant syndrome results from damage to both parietal lobes. Clinically, it includes three main symptoms: simultanagnosia (the inability to see more than one object at a time); optic ataxia (the fixation of gaze with severe problems in voluntarily moving fixation); and optic apraxia (the inability to reach towards the correct location of perceived objects" It can occur with dementia. Balint's syndrome lose spatial information outside their own bodies and are functionally blind except for the perception of one object in the visual scene at a time. Their spatial abilities are so impaired that they cannot locate the item they can perceive." Nature Reviews Neuroscience 2003 4, 93-102
Question 17
The Re-LY stroke trial examined the efficacy of dabigatran compared to warfarin in the prevention of thromboembolic stroke in patients who have atrial fibrillation. Which of the following results was not an outcome from that study?
(A) 110mg BD dabigatran and 150mg BD dabigatran showed a statistically significant decrease in risk of hemorrhagic stroke
(B) 110mg BD dabigatran showed a statistically significant decrease in major bleeding risk, whilst 150mg BD dabigatran showed a similar major bleeding risk when compared to warfarin
(C) 110mg BD dabigatran was found superior to warfarin in prevention of thromboembolic stroke
(D) 150mg BD dabigatran was found superior to warfarin in prevention of thromboembolic stroke
(E) 110mg BD dabigatran was non-inferior to warfarin in prevention of thromboembolic stroke
C: Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361:1139–1151.
Question 18
A 79-year-old man was admitted with a middle cerebral artery infarction confirmed by a CT scan of head. He was in atrial fibrillation and had no contraindications to starting warfarin. He made a good early recovery. What is the general recommended time to wait prior to starting anticoagulation therapy for this patient?
(A) 1 day
(B) 1 week
(C) 2 weeks
(D) 1 month
(E) 6 months
C: According to the Australian stroke guidelines 2010, the decision to anti coagulate can be delayed up to 2 weeks. The NICE guidelines suggest that one should wait 2 weeks prior to initiating anticoagulation.
Question 19
A 34 year old male presents acutely with quadraplegia and complete paralysis of his facial muscles. He is able to move his eyes and blink on command. Where is the most likely lesion?
(A) dorsal medulla
(B) Left cerebellum
(C) dorsal pons
(D) ventral pons
(E) reticular activating system
D: This is a case of locked in syndrome, which most frequently involves the ventral pons where the corticospinal tracts and corticobulbar tracts are concentrated.
Question 20
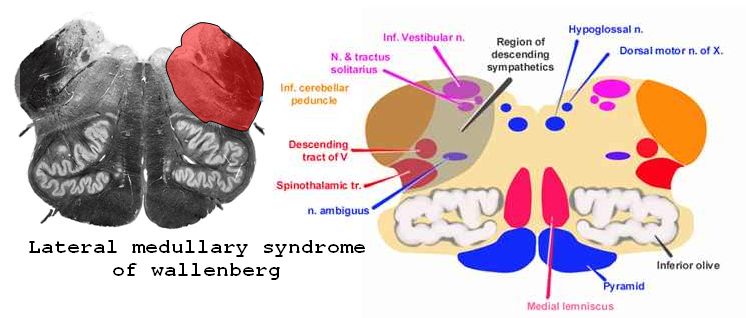
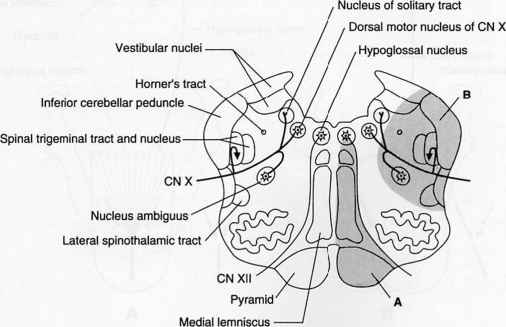
A 43 year old male presents after chiropractic neck manipulation with left sided horners syndrome, dysarthria, dysphagia, hoarseness, left sided facial nerve palsy and a right hemianaesthesia to pin prick and temperature. What is the most likely syndrome?
(A) Lateral medullary syndrome
(B) Medial medullary syndrome
(C) Ventral pontine syndrome
(D) Tip of the basilar syndrome
(E) Middle Cerebral artery infarct
A: The lateral medullary artery syndrome can occur with dissection of the vertebral artery or thrombus into the posterior inferior cerebellar artery. The infarcted tissue lies in the lateral medulla, including CNVIII vestibular nuclei, causing dizziness, CN 5 nucleus causing ipsilateral pain and temperature loss in face, dysphagia and hoarseness secondary to nucleus ambiguous (motor CNX) involvement, and contralateral pain and temperature loss secondary to lesions that are above the decussation point for the spinothalamic tract. Horner's syndrome occurs because of involvement of descending sympathetic tracts. Image below courtesy of medchrome.com
A 79-year-old man was admitted with a middle cerebral artery infarction confirmed by a CT scan of head. He was in atrial fibrillation and had no contraindications to starting warfarin. He made a good early recovery. What is the general recommended time to wait prior to starting anticoagulation therapy for this patient?
(A) 1 day
(B) 1 week
(C) 2 weeks
(D) 1 month
(E) 6 months
C: According to the Australian stroke guidelines 2010, the decision to anti coagulate can be delayed up to 2 weeks. The NICE guidelines suggest that one should wait 2 weeks prior to initiating anticoagulation.
Question 19
A 34 year old male presents acutely with quadraplegia and complete paralysis of his facial muscles. He is able to move his eyes and blink on command. Where is the most likely lesion?
(A) dorsal medulla
(B) Left cerebellum
(C) dorsal pons
(D) ventral pons
(E) reticular activating system
D: This is a case of locked in syndrome, which most frequently involves the ventral pons where the corticospinal tracts and corticobulbar tracts are concentrated.
Question 20
A 43 year old male presents after chiropractic neck manipulation with left sided horners syndrome, dysarthria, dysphagia, hoarseness, left sided facial nerve palsy and a right hemianaesthesia to pin prick and temperature. What is the most likely syndrome?
(A) Lateral medullary syndrome
(B) Medial medullary syndrome
(C) Ventral pontine syndrome
(D) Tip of the basilar syndrome
(E) Middle Cerebral artery infarct
A: The lateral medullary artery syndrome can occur with dissection of the vertebral artery or thrombus into the posterior inferior cerebellar artery. The infarcted tissue lies in the lateral medulla, including CNVIII vestibular nuclei, causing dizziness, CN 5 nucleus causing ipsilateral pain and temperature loss in face, dysphagia and hoarseness secondary to nucleus ambiguous (motor CNX) involvement, and contralateral pain and temperature loss secondary to lesions that are above the decussation point for the spinothalamic tract. Horner's syndrome occurs because of involvement of descending sympathetic tracts. Image below courtesy of medchrome.com
Question 21
A 96 year old male presents to the emergency department confused and disoriented. A neurological examination reveals that, despite him saying so, there is readily demonstrable blindness. When asked to name objects, he misnames them. What is the name given to this syndrome?
(A) Wallenbergs syndrome
(B) Josephs syndrome
(C) Sweets syndrome
(D) Anton's syndrome
(E) Gerstman's syndrome
D: Typically caused by bilateral lesions in the occipital lobes leading to a visual anasognosia
Question 22
A 84 year old male presents with weakness to Bathurst emergency department. A neurological examination reveals the patient to have left sided arm and leg weakness, right sided tongue fasciculation's and weakness with deviation to the left and left sided loss in light touch, vibration and proprioception. Where is the most likely lesion?
(A) Medial medulla
(B) Lateral medulla
(C) ventral pons
(D) dorsal pons
(E) internal capsule
A: This is an example of medial medullary syndrome. This is a rare neurological syndrome and occurs from infarctions involving the basilar artery or vertebral artery territory. The lateral medullary syndrome is much more common in aetiology. Neurology 1997 Apr;48(4):882-90. Image courtesy of vertigoexercisesus.com
A 96 year old male presents to the emergency department confused and disoriented. A neurological examination reveals that, despite him saying so, there is readily demonstrable blindness. When asked to name objects, he misnames them. What is the name given to this syndrome?
(A) Wallenbergs syndrome
(B) Josephs syndrome
(C) Sweets syndrome
(D) Anton's syndrome
(E) Gerstman's syndrome
D: Typically caused by bilateral lesions in the occipital lobes leading to a visual anasognosia
Question 22
A 84 year old male presents with weakness to Bathurst emergency department. A neurological examination reveals the patient to have left sided arm and leg weakness, right sided tongue fasciculation's and weakness with deviation to the left and left sided loss in light touch, vibration and proprioception. Where is the most likely lesion?
(A) Medial medulla
(B) Lateral medulla
(C) ventral pons
(D) dorsal pons
(E) internal capsule
A: This is an example of medial medullary syndrome. This is a rare neurological syndrome and occurs from infarctions involving the basilar artery or vertebral artery territory. The lateral medullary syndrome is much more common in aetiology. Neurology 1997 Apr;48(4):882-90. Image courtesy of vertigoexercisesus.com
Question 22
What is the quoted percentage of fatal intracranial haemorrhages that occur during the initial 7 days after the use of intravenous alteplase?
(A) 0.5%
(B) 1%
(C) 2%
(D) 5%
(E) 10%
C: " Alteplase significantly increased the odds of symptomatic intracranial haemorrhage (type 2 parenchymal haemorrhage definition 231 [6·8%] of 3391 vs 44 [1·3%] of 3365, OR 5·55, 95% CI 4·01-7·70, p<0·0001; SITS-MOST definition 124 [3·7%] vs 19 [0·6%], OR 6·67, 95% CI 4·11-10·84, p<0·0001) and of fatal intracranial haemorrhage within 7 days (91 [2·7%] vs 13 [0·4%]; OR 7·14, 95% CI 3·98-12·79, p<0·0001). The relative increase in fatal intracranial haemorrhage from alteplase was similar irrespective of treatment delay, age, or stroke severity, but the absolute excess risk attributable to alteplase was bigger among patients who had more severe strokes. There was no excess in other early causes of death and no significant effect on later causes of death. Consequently, mortality at 90 days was 608 (17·9%) in the alteplase group versus 556 (16·5%) in the control group (hazard ratio 1·11, 95% CI 0·99-1·25, p=0·07)." Lancet. 2014 Nov 29;384(9958):1929-35. doi: 10.1016/S0140-6736(14)60584-5. Epub 2014 Aug 5.
What is the quoted percentage of fatal intracranial haemorrhages that occur during the initial 7 days after the use of intravenous alteplase?
(A) 0.5%
(B) 1%
(C) 2%
(D) 5%
(E) 10%
C: " Alteplase significantly increased the odds of symptomatic intracranial haemorrhage (type 2 parenchymal haemorrhage definition 231 [6·8%] of 3391 vs 44 [1·3%] of 3365, OR 5·55, 95% CI 4·01-7·70, p<0·0001; SITS-MOST definition 124 [3·7%] vs 19 [0·6%], OR 6·67, 95% CI 4·11-10·84, p<0·0001) and of fatal intracranial haemorrhage within 7 days (91 [2·7%] vs 13 [0·4%]; OR 7·14, 95% CI 3·98-12·79, p<0·0001). The relative increase in fatal intracranial haemorrhage from alteplase was similar irrespective of treatment delay, age, or stroke severity, but the absolute excess risk attributable to alteplase was bigger among patients who had more severe strokes. There was no excess in other early causes of death and no significant effect on later causes of death. Consequently, mortality at 90 days was 608 (17·9%) in the alteplase group versus 556 (16·5%) in the control group (hazard ratio 1·11, 95% CI 0·99-1·25, p=0·07)." Lancet. 2014 Nov 29;384(9958):1929-35. doi: 10.1016/S0140-6736(14)60584-5. Epub 2014 Aug 5.