Question 1
What is the importance of the P1 receptor present on mast cells and eosinophils?
(A) It induces differentiation
(B) it induces degranulation
(C) It induces apoptosis
(D) It activates Calcium channels
(E) It activates ligand gated sodium channels
C: adenosine is an endogenous ligand for the receptor, and it is a g-protein coupled receptor
Question 2
A 29 year old lawyer from Brisbane presents with recurrent soft cutaneous tissue swelling, lip swelling and shortness of breath with a choking sensation. Her mother and her mother's twin sister both had a similar condition. She is currently hypotensive and has a respiratory rate of 40, saturating at 92% on room air. Apart from instituting fluid resuscitation and fluid therapy, and assuming the patient is in a tertiary referral centre, what is the most appropriate management step?
(A) IV adrenaline
(B) IM adrenaline
(C) hydrocortisone and promethazine
(D) fresh frozen plasma
(E) C1-esterase inhibitor concentrate
E: hereditary angioedema occurs due to a deficiency of C1 esterase inhibitor, and lack of inhibitors leads to uncontrolled activation of C1 and therefore consumption of C4 and C2. Complement mediators lead to release of vasoactive mediators such as kinins. C3 is not decreased as it is controlled through other means. The way in which kinins are involved in this pathogenesis is through C2 --> C2b (which is acted on by plasmin) to become C2-kinin. This process is normally inhibited by C1-INH. To test, require C4, C3 levels as well as levels of C1-INH and C1-INH activity. Type 1 is due to decreased production of C1-INH, type 2 is due to decreased function of the protein. Acquired angioedema may also occur and are typically associated with B-lymphoproliferative disorders secondary to the consumption of C1-INH. Adrenaline has no use in this syndrome, and C1-esteralse inhibitor concentrate should be used. If not available, then FFP is an alternative. Immunology4bpts course. Immunobiology 1998; 199:377. Allergy Asthma Clin Immunol 2010; 6:20.
Question 3
Which of the following complement components is the most potent anaphylatoxin and chemotactic factor?
(A) C5a
(B) C4a
(C) C3a
(D) C3b
(E) C4b
A: C5a > C3a >>C4a. They are designed to act locally to facilitate acute inflammation and when released in excess they can mediate anaphylactic shock.
Question 4
What is the mechanism of ACE-inhibitor induced angioedema
(A) ACE-inhibitor related direct degranulation of mast cells
(B) ACE-inhibitor induced direct degranulation of eosinophils
(C) ACE-inhibitor related inhibition of complement regulation factor H
(D) ACE-inhibitor related decline in degradation of bradykinin
(E) ACE-inhibitor related direct activation of bradykinin 2 receptor
D: Lancet. 1998;351(9117):1693.
Question 5
Icatibant has recently shown efficacy in the treatment of ACE-inhibitor induced angioedema and in hereditary angioedema. What is its mechanism of action?
(A) Inhibition of bradykinin 2 receptor
(B) Degradation of bradykinin 1 receptor
(C) down regulation of H1,2 and 3 receptors
(D) mast cell stabiliser
(E) inhibition of MAPK
A: icatibant is a selective B2 bradykinin receptor antagonist, and has shown efficacy in the treatment of ACE-inhibitor related angioedema. "Among patients with ACE-inhibitor–induced angioedema, the time to complete resolution of edema was significantly shorter with icatibant than with combination therapy with a glucocorticoid and an antihistamine". "The median time to complete resolution was 8.0 hours (interquartile range, 3.0 to 16.0) with icatibant as compared with 27.1 hours (interquartile range, 20.3 to 48.0) with standard therapy (P=0.002)". N Engl J Med 2015; 372:418-425
Question 6
Which of the following immunoglobulin subtypes is MOST potent at activating complement?
(A) IgG3
(B) IgG1
(C) IgM
(D) IgG2
(E) IgG4
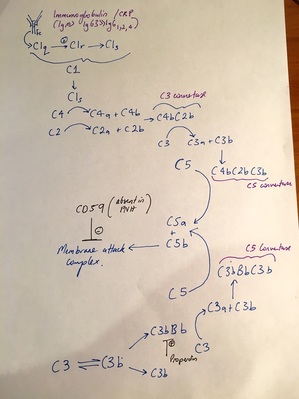
C: IgM is a pentameric structure and is the most potent at activating complement. The CH2 domain is able to bind to C1q, changing its conformation and causing C1r to auto-catalyse its own cleavage. This activated C1r then activates C1s. It is eventually C1s that cleaves C4 and C2 into C4bC2b, which is the classical pathway C3 convertase. In terms of potency, IgM > IgG3 > IgG1 > IgG2 >>IgG4 N Engl J Med 2001; 344:1058. N Engl J Med 2001; 344:1140.
Question 7
What is the mechanism of Eculizumab?
(A) Inhibits C3 converts
(B) Inhibits C5 converts
(C) Inhibits C5
(D) Inhibits C4
(E) Inhibits C9
C: Eculizumab, which has shown evidence for its use in PNH and atypical HUS, inhibits the terminal complement protein C5. Intravascular hemolysis is a prominent feature of PNH and is the consequence of the absence of the GPI-linked complement regulatory protein CD59. CD59 blocks the formation of the terminal complement complex (also called the membrane-attack complex) on the cell surface, thereby preventing erythrocyte lysis and in vitro platelet activation N Engl J Med 2006; 355:1233-1243; N Engl J Med 2013; 368:2169-2181
Question 8
What is false about the alternate pathway of complement action?
(A) C3 is constantly ticking over to form C3b
(B) C3b can be stabilised on microbial surfaces or if free reacts with water to form C3(H2O) and is eventually degraded
(C) C3bBb is the alternative pathway C3 convertase
(D) C3bBb is stabilised by mannose binding lectin
(E) C3bBbC3b is the alternative pathway C5 convertase
D: C3bBb is stabilised by properdin. There is a rare X-linked deficiency of properdin, leading to fulminant meningococcal septicaemia. The alternative complement pathway is activated by microbial cell stabilisation of C3b. Factor D is able to allow the bound factor B on C3bB --> C3bBb. This is subsequently stabilised by properdin, and is the alternate pathway C3 convertase. The classical (and mannose binding lectin) pathway C3 convertase is C4bC2b. The C3 convertase catalyses C3 --> C3a + C3b, and the alternate pathway C5 convertase is C3bBbC3b, whilst the classical complement (and mannose binding lectin) component C5 convertase is C4bC2bC3b. The C5 convertase catalyses C5 --> C5a + C5b, where C5a is a potent chemokine and anaphylatoxin. Nat Rev Immunol 2009; 9:729.
What is the importance of the P1 receptor present on mast cells and eosinophils?
(A) It induces differentiation
(B) it induces degranulation
(C) It induces apoptosis
(D) It activates Calcium channels
(E) It activates ligand gated sodium channels
C: adenosine is an endogenous ligand for the receptor, and it is a g-protein coupled receptor
Question 2
A 29 year old lawyer from Brisbane presents with recurrent soft cutaneous tissue swelling, lip swelling and shortness of breath with a choking sensation. Her mother and her mother's twin sister both had a similar condition. She is currently hypotensive and has a respiratory rate of 40, saturating at 92% on room air. Apart from instituting fluid resuscitation and fluid therapy, and assuming the patient is in a tertiary referral centre, what is the most appropriate management step?
(A) IV adrenaline
(B) IM adrenaline
(C) hydrocortisone and promethazine
(D) fresh frozen plasma
(E) C1-esterase inhibitor concentrate
E: hereditary angioedema occurs due to a deficiency of C1 esterase inhibitor, and lack of inhibitors leads to uncontrolled activation of C1 and therefore consumption of C4 and C2. Complement mediators lead to release of vasoactive mediators such as kinins. C3 is not decreased as it is controlled through other means. The way in which kinins are involved in this pathogenesis is through C2 --> C2b (which is acted on by plasmin) to become C2-kinin. This process is normally inhibited by C1-INH. To test, require C4, C3 levels as well as levels of C1-INH and C1-INH activity. Type 1 is due to decreased production of C1-INH, type 2 is due to decreased function of the protein. Acquired angioedema may also occur and are typically associated with B-lymphoproliferative disorders secondary to the consumption of C1-INH. Adrenaline has no use in this syndrome, and C1-esteralse inhibitor concentrate should be used. If not available, then FFP is an alternative. Immunology4bpts course. Immunobiology 1998; 199:377. Allergy Asthma Clin Immunol 2010; 6:20.
Question 3
Which of the following complement components is the most potent anaphylatoxin and chemotactic factor?
(A) C5a
(B) C4a
(C) C3a
(D) C3b
(E) C4b
A: C5a > C3a >>C4a. They are designed to act locally to facilitate acute inflammation and when released in excess they can mediate anaphylactic shock.
Question 4
What is the mechanism of ACE-inhibitor induced angioedema
(A) ACE-inhibitor related direct degranulation of mast cells
(B) ACE-inhibitor induced direct degranulation of eosinophils
(C) ACE-inhibitor related inhibition of complement regulation factor H
(D) ACE-inhibitor related decline in degradation of bradykinin
(E) ACE-inhibitor related direct activation of bradykinin 2 receptor
D: Lancet. 1998;351(9117):1693.
Question 5
Icatibant has recently shown efficacy in the treatment of ACE-inhibitor induced angioedema and in hereditary angioedema. What is its mechanism of action?
(A) Inhibition of bradykinin 2 receptor
(B) Degradation of bradykinin 1 receptor
(C) down regulation of H1,2 and 3 receptors
(D) mast cell stabiliser
(E) inhibition of MAPK
A: icatibant is a selective B2 bradykinin receptor antagonist, and has shown efficacy in the treatment of ACE-inhibitor related angioedema. "Among patients with ACE-inhibitor–induced angioedema, the time to complete resolution of edema was significantly shorter with icatibant than with combination therapy with a glucocorticoid and an antihistamine". "The median time to complete resolution was 8.0 hours (interquartile range, 3.0 to 16.0) with icatibant as compared with 27.1 hours (interquartile range, 20.3 to 48.0) with standard therapy (P=0.002)". N Engl J Med 2015; 372:418-425
Question 6
Which of the following immunoglobulin subtypes is MOST potent at activating complement?
(A) IgG3
(B) IgG1
(C) IgM
(D) IgG2
(E) IgG4
C: IgM is a pentameric structure and is the most potent at activating complement. The CH2 domain is able to bind to C1q, changing its conformation and causing C1r to auto-catalyse its own cleavage. This activated C1r then activates C1s. It is eventually C1s that cleaves C4 and C2 into C4bC2b, which is the classical pathway C3 convertase. In terms of potency, IgM > IgG3 > IgG1 > IgG2 >>IgG4 N Engl J Med 2001; 344:1058. N Engl J Med 2001; 344:1140.
Question 7
What is the mechanism of Eculizumab?
(A) Inhibits C3 converts
(B) Inhibits C5 converts
(C) Inhibits C5
(D) Inhibits C4
(E) Inhibits C9
C: Eculizumab, which has shown evidence for its use in PNH and atypical HUS, inhibits the terminal complement protein C5. Intravascular hemolysis is a prominent feature of PNH and is the consequence of the absence of the GPI-linked complement regulatory protein CD59. CD59 blocks the formation of the terminal complement complex (also called the membrane-attack complex) on the cell surface, thereby preventing erythrocyte lysis and in vitro platelet activation N Engl J Med 2006; 355:1233-1243; N Engl J Med 2013; 368:2169-2181
Question 8
What is false about the alternate pathway of complement action?
(A) C3 is constantly ticking over to form C3b
(B) C3b can be stabilised on microbial surfaces or if free reacts with water to form C3(H2O) and is eventually degraded
(C) C3bBb is the alternative pathway C3 convertase
(D) C3bBb is stabilised by mannose binding lectin
(E) C3bBbC3b is the alternative pathway C5 convertase
D: C3bBb is stabilised by properdin. There is a rare X-linked deficiency of properdin, leading to fulminant meningococcal septicaemia. The alternative complement pathway is activated by microbial cell stabilisation of C3b. Factor D is able to allow the bound factor B on C3bB --> C3bBb. This is subsequently stabilised by properdin, and is the alternate pathway C3 convertase. The classical (and mannose binding lectin) pathway C3 convertase is C4bC2b. The C3 convertase catalyses C3 --> C3a + C3b, and the alternate pathway C5 convertase is C3bBbC3b, whilst the classical complement (and mannose binding lectin) component C5 convertase is C4bC2bC3b. The C5 convertase catalyses C5 --> C5a + C5b, where C5a is a potent chemokine and anaphylatoxin. Nat Rev Immunol 2009; 9:729.
Question 9
What is the most common time frame that ACE-inhibitor associated angioedema occurs?
(A) 1 day from initiation
(B) 1 week from initiation
(C) 1 month from initiation
(D) 1 year from initiation
(E) 10 years from initiation
B: Reports of up to 1 year delay have been described. Prevalence is 1:1000. N Engl J Med 2015; 372:1866-1868
Question 10
What cut-off is generally considered significant for ANA +
(A) 1:80
(B) 1:160
(C) 1:256
(D) 1:2560
(E) 1:3880
B: RPA course, note 20% of adults, especially females may have ANA +
Question 11
Which of the following is NOT a target of ANCA?
(A) Cathepsin G
(B) Lactoferrin
(C) myeloperoxidase
(D) Lactate dehydrogenase
(E) proteinase-3
D: N Engl J Med 1997; 337:1512-1523, RPA Course 2015, RPA lectures 2015 - Elastase, bacterial permeability increasing factor are other ANCA targets. ANCA is detected through dissolving neutrophil membranes with ethanol, and watching certain antigens stay in cytoplasm (c-anca = PR3) or watching other antigens (which are cationic) migrate to the nucleus (which is anionic, p-anca = mpo).
Question 12
Which of the following antiphospholipid antibodies is associated with the greatest risk of thrombosis?
(A) IgG anticardiolipin (IgG2)
(B) IgM anticardiolipin
(C) anti-beta2glycoprotein1
(D) lupuas anticoagulant
(E) ANA
A: RPA Course 2015
Question 13
Which of the following is not a major protein fraction seperated by zone electrophoresis?
(A) Albumin
(B) alpha-1 globulins
(C) alpha-2 globulins
(D) beta globulins
(E) delta globulins
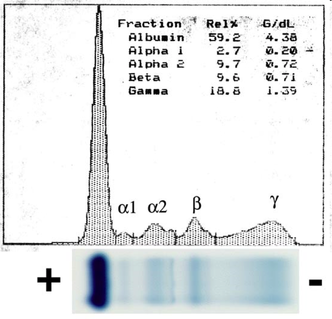
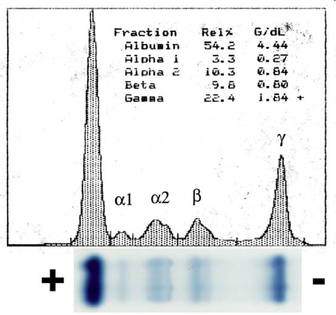
E: No such thing as delta globulins on EPG, gamma globulins are present, this is where the M protein is detected and quantified using densitometry. The first picture is a normal EPG and the second picture denotes a paraprotein. The process of immunofixation EPG involves multiple wells, whereby the patients serum is run on a number of different wells, with a control, following by the addition of precipitating antibodies (IgG, A, M, E, G, kappa, Lamda) to detect the type.
What is the most common time frame that ACE-inhibitor associated angioedema occurs?
(A) 1 day from initiation
(B) 1 week from initiation
(C) 1 month from initiation
(D) 1 year from initiation
(E) 10 years from initiation
B: Reports of up to 1 year delay have been described. Prevalence is 1:1000. N Engl J Med 2015; 372:1866-1868
Question 10
What cut-off is generally considered significant for ANA +
(A) 1:80
(B) 1:160
(C) 1:256
(D) 1:2560
(E) 1:3880
B: RPA course, note 20% of adults, especially females may have ANA +
Question 11
Which of the following is NOT a target of ANCA?
(A) Cathepsin G
(B) Lactoferrin
(C) myeloperoxidase
(D) Lactate dehydrogenase
(E) proteinase-3
D: N Engl J Med 1997; 337:1512-1523, RPA Course 2015, RPA lectures 2015 - Elastase, bacterial permeability increasing factor are other ANCA targets. ANCA is detected through dissolving neutrophil membranes with ethanol, and watching certain antigens stay in cytoplasm (c-anca = PR3) or watching other antigens (which are cationic) migrate to the nucleus (which is anionic, p-anca = mpo).
Question 12
Which of the following antiphospholipid antibodies is associated with the greatest risk of thrombosis?
(A) IgG anticardiolipin (IgG2)
(B) IgM anticardiolipin
(C) anti-beta2glycoprotein1
(D) lupuas anticoagulant
(E) ANA
A: RPA Course 2015
Question 13
Which of the following is not a major protein fraction seperated by zone electrophoresis?
(A) Albumin
(B) alpha-1 globulins
(C) alpha-2 globulins
(D) beta globulins
(E) delta globulins
E: No such thing as delta globulins on EPG, gamma globulins are present, this is where the M protein is detected and quantified using densitometry. The first picture is a normal EPG and the second picture denotes a paraprotein. The process of immunofixation EPG involves multiple wells, whereby the patients serum is run on a number of different wells, with a control, following by the addition of precipitating antibodies (IgG, A, M, E, G, kappa, Lamda) to detect the type.
Question 14
Which of the following is NOT a live attenuated vaccine?
(A) MMR
(B) Oral Polio
(C) BCG
(D) Yellow Fever
(E) Hepatitis A
E: Live attenuated vaccines --> MOBY VRT (MMR, oral Polio, BCG, YF, varicella Zoster, Rabies, Oral typhoid). Contraindicated if on anti-TB meds, HIV with CD4 < 200, Prednisolone > 20mg. Suggested that patients either obtain these meds 3 weeks prior to or wait 3 months after the drugs are given (3 month wash out period prior to vaccine). RPA Course 2015, PEP 2014
Question 15
Interferon gamma and IL-2 are involved in the conversion of Th0 cells to which subtype?
(A) Th1
(B) Th2
(C) TReg
(D) Th17
(E) Th4
A
Question 16
IL4, IL5 and IL13 are involved in the conversion of Th0 cells to which subtype?
(A) Th1
(B) Th2
(C) TReg
(D) Th17
(E) Th4
B
Question 17
IL17, IL21 and IL22 are involved in the conversion of Th0 cells to which subtype?
(A) Th1
(B) Th2
(C) TReg
(D) Th17
(E) Th4
D
Question 18
IL10 and TGF-beta are involved in the conversion of Th0 cells to which subtype?
(A) Th1
(B) Th2
(C) TReg
(D) Th17
(E) Th4
C
Question 19
With regards to transplant immunology?
(A) The direct pathway involves the presentation of donor antigens on donor APCs to recipient T cells with subsequent activation
(B) The indirect pathway involves the presentation of recipient antigens to donor T cells
(C) The direct pathway involves the direct toxicity of T cells on graft without the involvement of donor or recipient APCs
(D) CTLA4 blockade represents a powerful tool in suppressing T cell activation
(E) Anti-TNF-alpha antigens are powerful immunosupressents that are currently being utilised in clinical practice in kidney and pancreas combined transplants
A: The indirect pathway refers to recipient APCs presenting donor antigens to recipient T cells.
Question 20
What is FALSE regarding co-stimulatory molecules?
(A) CD80 and CD86 on antigen presenting cells have affinity to CD28 and CTLA-4 on T cells
(B) CD80 and CD86 have higher affinity for CTLA-4 than CD28
(C) Belatacept is a combination of CTLA-4 with Fc, thus blocking CD80 and CD86 binding to CD28, preventing co-stimulation activation
(D) CD40:CD40L interaction is an important co-stimulator
(E) CD3 interaction with Fox-P3 receptor alpha decreases T cell activation
E: This is entirely made up by me!
Question 21
Which of the following is FALSE concerning the mecahism of acute cellular rejection
(A) Effector CD8 T cells migrate through into the interstitium where they mediate acute cellular rejection
(B) Fas Ligand pathway activates caspase mediated apoptosis in graft cells
(C) Deletion of interferon gamma genes protects against acute cellular rejection in animal models
(D) Granzymes released by CD8 T cells activate the caspase mediated apoptosis pathway in graft cells
(E) Perforins released by CD8 T cells are able to form pores on cells leading to cell lysis
C: Paradoxical! RPA Course 2015
Which of the following is NOT a live attenuated vaccine?
(A) MMR
(B) Oral Polio
(C) BCG
(D) Yellow Fever
(E) Hepatitis A
E: Live attenuated vaccines --> MOBY VRT (MMR, oral Polio, BCG, YF, varicella Zoster, Rabies, Oral typhoid). Contraindicated if on anti-TB meds, HIV with CD4 < 200, Prednisolone > 20mg. Suggested that patients either obtain these meds 3 weeks prior to or wait 3 months after the drugs are given (3 month wash out period prior to vaccine). RPA Course 2015, PEP 2014
Question 15
Interferon gamma and IL-2 are involved in the conversion of Th0 cells to which subtype?
(A) Th1
(B) Th2
(C) TReg
(D) Th17
(E) Th4
A
Question 16
IL4, IL5 and IL13 are involved in the conversion of Th0 cells to which subtype?
(A) Th1
(B) Th2
(C) TReg
(D) Th17
(E) Th4
B
Question 17
IL17, IL21 and IL22 are involved in the conversion of Th0 cells to which subtype?
(A) Th1
(B) Th2
(C) TReg
(D) Th17
(E) Th4
D
Question 18
IL10 and TGF-beta are involved in the conversion of Th0 cells to which subtype?
(A) Th1
(B) Th2
(C) TReg
(D) Th17
(E) Th4
C
Question 19
With regards to transplant immunology?
(A) The direct pathway involves the presentation of donor antigens on donor APCs to recipient T cells with subsequent activation
(B) The indirect pathway involves the presentation of recipient antigens to donor T cells
(C) The direct pathway involves the direct toxicity of T cells on graft without the involvement of donor or recipient APCs
(D) CTLA4 blockade represents a powerful tool in suppressing T cell activation
(E) Anti-TNF-alpha antigens are powerful immunosupressents that are currently being utilised in clinical practice in kidney and pancreas combined transplants
A: The indirect pathway refers to recipient APCs presenting donor antigens to recipient T cells.
Question 20
What is FALSE regarding co-stimulatory molecules?
(A) CD80 and CD86 on antigen presenting cells have affinity to CD28 and CTLA-4 on T cells
(B) CD80 and CD86 have higher affinity for CTLA-4 than CD28
(C) Belatacept is a combination of CTLA-4 with Fc, thus blocking CD80 and CD86 binding to CD28, preventing co-stimulation activation
(D) CD40:CD40L interaction is an important co-stimulator
(E) CD3 interaction with Fox-P3 receptor alpha decreases T cell activation
E: This is entirely made up by me!
Question 21
Which of the following is FALSE concerning the mecahism of acute cellular rejection
(A) Effector CD8 T cells migrate through into the interstitium where they mediate acute cellular rejection
(B) Fas Ligand pathway activates caspase mediated apoptosis in graft cells
(C) Deletion of interferon gamma genes protects against acute cellular rejection in animal models
(D) Granzymes released by CD8 T cells activate the caspase mediated apoptosis pathway in graft cells
(E) Perforins released by CD8 T cells are able to form pores on cells leading to cell lysis
C: Paradoxical! RPA Course 2015